CHC2017:TAVR 会成为主动脉瓣疾病主要手段吗?
2017-08-11 佚名 中国循环杂志
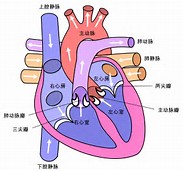
在昨天进行的结构性心脏病论坛上,来自德国的瓣膜介入治疗先驱Eberhard Grube 教授和阜外医院杨跃进教授对经导管主动脉瓣置换术(TAVR)临床治疗现状及进展做了精彩报告。Grube 教授认为,TAVR 的很多问题已得到了较好的解决,随着技术的进一步进展,临床研究数据的进一步完善,TAVR 有望成为主动脉瓣疾病患者的主要治疗选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#AVR#
73
#主动脉瓣#
90
#主动脉#
71
#主动脉瓣疾病#
68
#CHC#
0
学习了,好文章
102
非常好的文章,学习了,很受益
93