近红外光免疫疗法(NIR-PIT):治疗恶性胸膜间皮瘤的曙光
2020-06-22 Allan MedSci原创
NIR-PIT是一种安全的光疗法,可以靶向受肿瘤影响的区域。
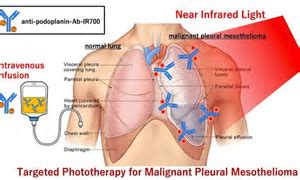
恶性胸膜间皮瘤(MPM)是一种罕见肿瘤,会影响肺内膜。MPM很少扩散到身体的其他部位,但通常患者被确诊时已处于晚期,导致预后不良和治疗选择非常有限。日本名古屋大学Kazuhide Sato及其同事研究了近红外光免疫疗法(NIR-PIT)治疗MPM的有效性。NIR-PIT已被美国FDA快速批准用于治疗一种恶性头颈部肿瘤。为了使NIR-PIT起作用,必须首先注射靶向肿瘤细胞的化合物。该化合物由靶向癌细胞上特定结构的抗体和称为IR700的光吸收剂组成。当近红外光照射到受癌症影响的身体部位时,该化合物聚集在癌细胞膜上,导致急性细胞破裂和肿瘤死亡。
为了使NIR-PIT用于MPM,科学家需要一种专门针对MPM癌细胞的化合物。他们将注意力集中在一种名为NZ-1的抗体上,该抗体能够靶向跨膜糖蛋白Podoplanin的特定部分。Podoplanin通常存在于人体的许多细胞类型中,但在某些类型的癌细胞(包括MPM)中尤其丰富。
Kazuhide Sato表示:“肺和胸腔含有大量空气,因此可以有效地传输近红外光。NIR-PIT是一种安全的光疗法,可以靶向受肿瘤影响的区域。在没有近红外光照射的情况下,抗体-IR700偶联物对人体是无毒的”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#曙光#
69
#近红外#
72
#胸膜#
73
#间皮瘤#
77
学习了
143