Laryngoscope:鼻炎的冷冻手术消融治疗:一项前瞻性多中心研究的两年结果
2021-03-23 AlexYang MedSci原创
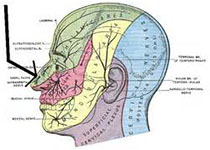
最近,有研究人员评估了鼻后神经冷冻消融治疗慢性鼻炎的长期(12-24个月)安全性和有效性情况。
最近,有研究人员评估了鼻后神经冷冻消融治疗慢性鼻炎的长期(12-24个月)安全性和有效性情况。 研究是一个多中心、前瞻性和单臂临床研究。研究在2017年2月到2020年4月之间进行。研究终点包括反映总鼻症状评分(rTNSS)、鼻结膜炎生活质量问卷(RQLQ)、医生使用临床整体印象-改善(CGI-I)评估改善情况的基线变化,以及治疗相关不良事件的发生率。 研究共有91名参与者在起始的12个月研究期间完成了研究。62名参与者同意长期随访,57人完成了24个月的随访。总rTNSS的显著改善反映在所有时间点与基线的中位数相比变化为-3.0或-4.0(P<0.001)。在所有随访中,超过80.0%的参与者在rTNSS上实现了至少≥1分的临床重要差异(MCID)改善。RQLQ总分表明生活质量有显著改善(P<0.0001)。超过77%的参与者达到了RQLQ总分的MCID(≥0.5分)。根据CGI-I,除了12个月的访问(61.9%)外,≥83.0%的人在所有的随访中都有改善。1名参与者经历了两起与治疗相关的严重不良事件。23名参与者共报告了29例不严重的治疗相关的AEs;大多数事件是短暂
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前瞻性#
66
#PE#
64
#多中心研究#
83
#多中心#
63
#消融#
66
#消融治疗#
89