Eur Urol Focus:前列腺活检与前列腺钬激光剜除术之间的短时间间隔与较差的围手术期结果有关
2021-04-25 AlexYang MedSci原创
目前还没有关于经直肠前列腺活检(PB)和前列腺钬激光切除术(HoLEP)之间的时间间隔对围手术期结果影响的数据。
目前还没有关于经直肠前列腺活检(PB)和前列腺钬激光切除术(HoLEP)之间的时间间隔对围手术期结果影响的数据。

最近,有研究人员评估了从PB到HoLEP的时间间隔对围手术期结果的影响。
研究包括了两个三级中心的172名连续的患者,他们在12个月内接受了HoLEP治疗,这些患者在手术之前曾接受过一次经直肠PB。研究结果发现,有93名(54%)和79名(46%)患者在HoLEP之前进行PB的时间分别为PB≤6和>6个月。PB≤6个月的患者出现术中并发症的比例高于PB>6个月的患者(14% vs 2.6%,p=0.04)。在多变量分析中,PB和HoLEP之间的时间间隔是术中并发症的独立预测因素(OR:0.74;95%CI:0.6-0.9;p=0.006)。从PB到HoLEP每多一个月,术中并发症的风险就会减少1.5%,切除效率增加4.1%,切除时间减少1.7分钟(所有P≤0.006)。研究的限制为选择之前只有一次PB的患者。
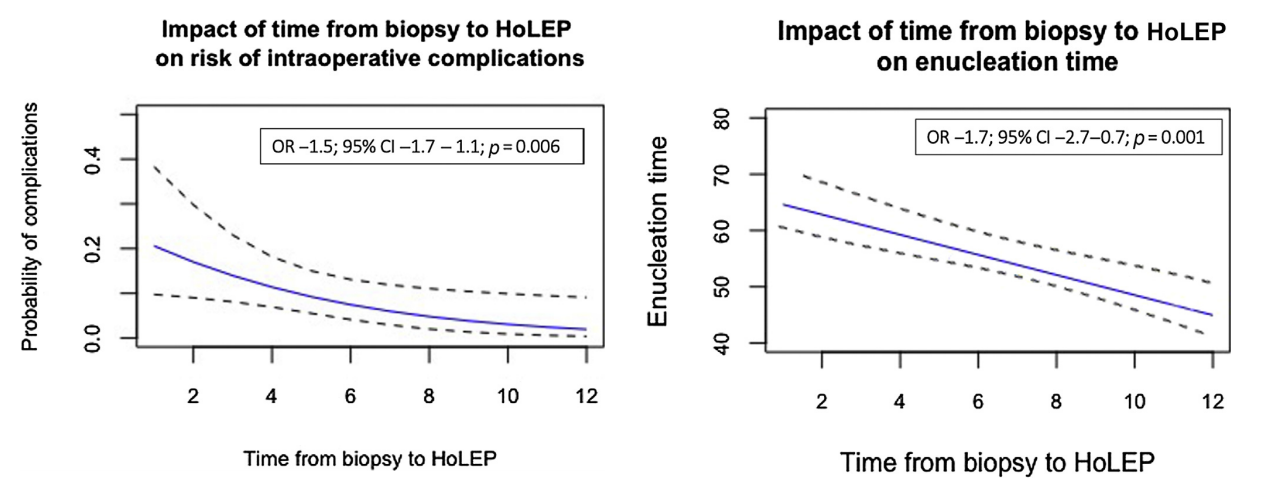
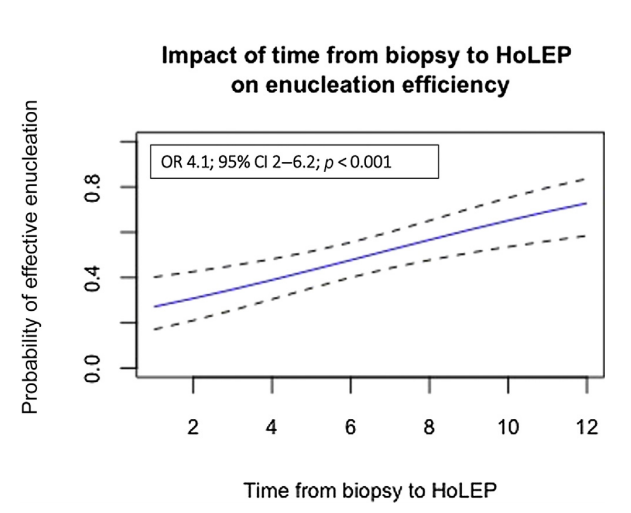
最后,研究人员指出,从PB到HoLEP的时间≤6个月与较高的术中并发症风险、较低的摘除疗效和较长的摘除时间有关。
原始出处:
Pietro Piazza , Lorenzo Bianchi , Marco Giampaoli et al. Short Time Delay Between Previous Prostate Biopsy for Prostate Cancer Assessment and Holmium Laser Enucleation of the Prostate Correlates with Worse Perioperative Outcomes. Eur Urol Focus. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#手术期#
57
#前列腺活检#
49
感谢分享
68
#活检#
50
#激光#
39