Prostate:抑制STAT3可防止体内前列腺癌的骨转移
2021-04-21 AlexYang MedSci原创
前列腺癌(PC)转移到骨骼会形成以硬化为主的病变,目前对骨转移性疾病还没有治愈的办法。转录因子信号转导和转录激活因子3(STAT3)认为是转移的驱动因素,但它作为骨转移的治疗靶点的潜力还没有研究。
前列腺癌(PC)转移到骨骼会形成以硬化为主的病变,目前对骨转移性疾病还没有治愈的办法。转录因子信号转导和转录激活因子3(STAT3)认为是转移的驱动因素,但它作为骨转移的治疗靶点的潜力还没有研究。

最近,有研究人员首次评估了STAT3抑制剂Napabucasin作为骨转移性PC治疗方案的情况。

研究结果发现,小分子STAT3抑制剂Stattic和Napabucasin都有效地削弱了PC细胞在体外的转移能力。此外,用Napabucasin治疗可以防止体内胫骨转移形成,也可以防止媒介处理VCaP异种移植中观察到的肿瘤引起的硬化骨反应。另外,用Napabucasin治疗已形成的骨CRPC,与媒介处理的动物相比,肿瘤负担和肿瘤引起的骨小梁体积都明显下降。与媒介处理的异种移植物相比,Napabucasin治疗的异种移植物的Ki67染色减少,证实了其抗有丝分裂的作用。基因表达量分析显示,股骨骨髓(BM)生态位的基因表达发生了变化,以维护造血干细胞和髓系。更多的是,Napabucasin处理的小鼠BM中红细胞数量的大幅增加。此外,在使用几种不同PC细胞系的骨异种移植模型中,免疫组化显示了肿瘤细胞周围的成骨细胞/骨膜细胞中STAT3磷酸化具有独特的模式。
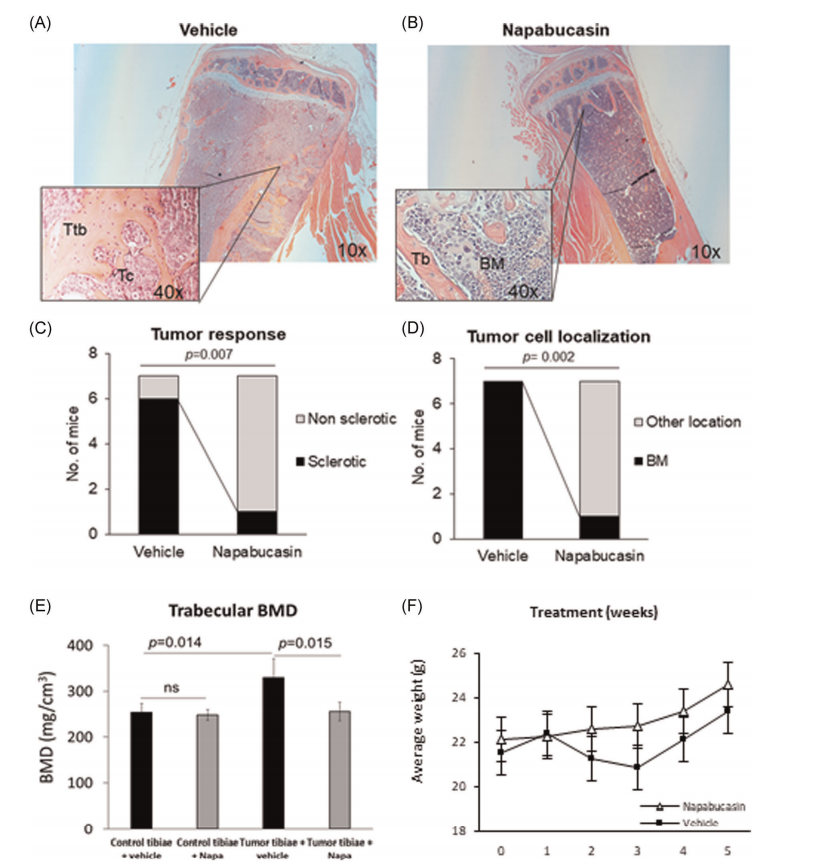
靶向STAT3可防止前列腺癌细胞的骨转移和减弱成骨细胞响应
最后,研究人员指出,抑制STAT3的活性会破坏骨转移的生态位,并同时靶向小鼠PC的骨骼建立和晚期骨转移CRPC,表明STAT3是骨骼转移性疾病的分子靶向治疗候选靶标。
原始出处:
Malin Hagberg Thulin, Jorma Määttä, Anna Linder et al. Inhibition of STAT3 prevents bone metastatic progression of prostate cancer in vivo. Prostate. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#STAT3#
59
#ROS#
47
#PRO#
50
前列腺癌相关研究,学习了,谢谢梅斯
71