NEJM:氨甲环酸在接受非心脏手术患者中的疗效
2022-05-27 MedSci原创 MedSci原创
在接受非心脏手术的患者中,氨甲环酸组的复合出血结局发生率显著低于安慰剂组。虽然复合心血管结局的组间差异很小,但氨甲环酸的非劣效性尚未明确。
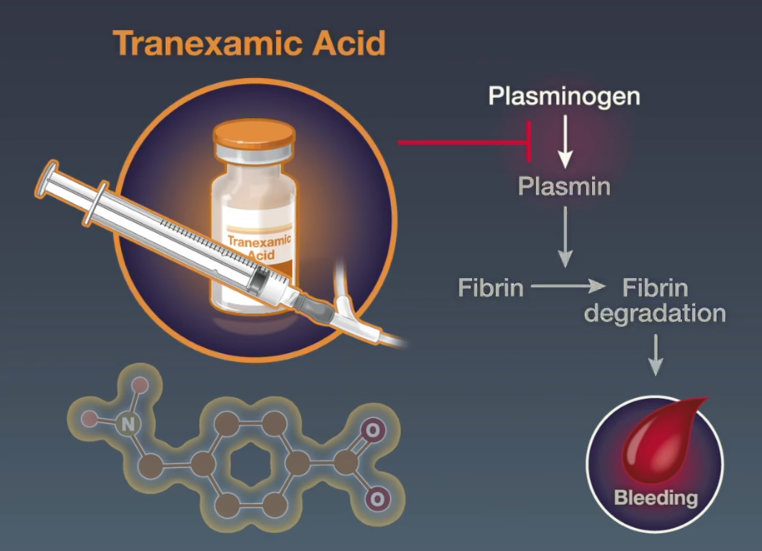
围手术期出血在接受非心脏手术的患者中很常见。氨甲环酸是一种抗纤溶药物,可以有效且安全地减少这种出血。
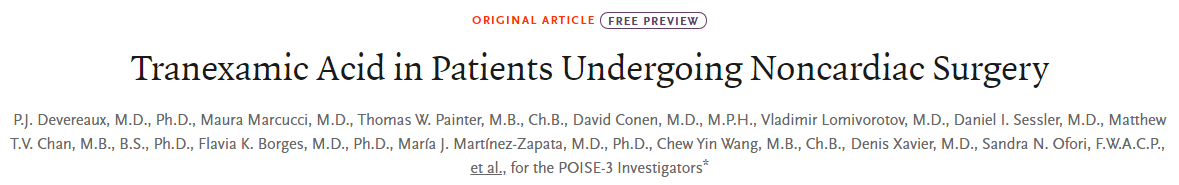
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员对接受非心脏手术的病人进行了试验。患者被随机分配在手术开始和结束时接受氨甲环酸(静脉注射1g)或安慰剂。
该研究的主要疗效结果为30天危及生命的出血、大出血或血液进入关键器官(复合出血结局)。该研究的主要安全性结局为30天后非心脏手术后心肌损伤、非出血性卒中、外周动脉血栓形成或症状性近端静脉血栓栓塞(复合心血管结局)。为了明确氨甲环酸与安慰剂在复合心血管结局方面的非劣效性,风险比的单侧97.5%置信区间的上限必须小于1.125,单侧P值必须小于0.025。
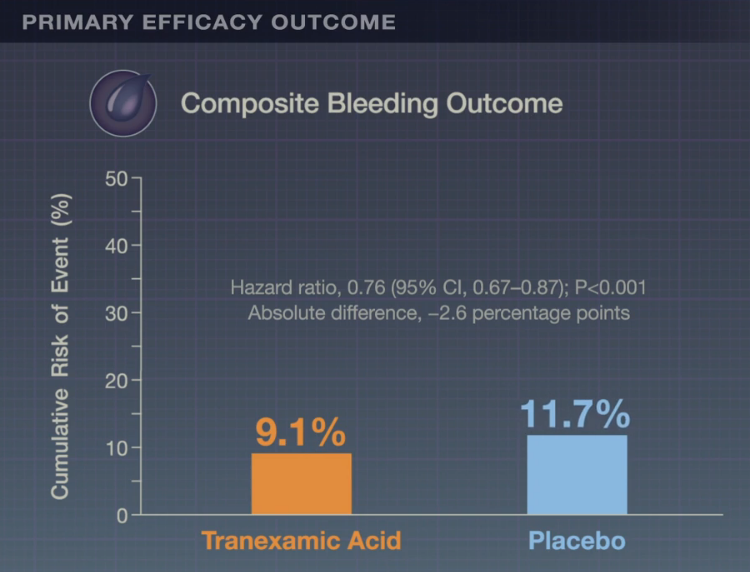
该研究共有9535名患者接受了随机分组。氨甲环酸组4757例患者中有433例(9.1%)患者发生了复合出血结局事件,安慰剂组4778例患者中有561例(11.7%)患者发生复合出血结局事件(风险比为0.76;95%置信区间[CI]为0.67~0.87;绝对差异为−2.6个百分点;95%CI为-3.8至-1.4;优势双侧P<0.001)。氨甲环酸组4581例患者中有649例(14.2%)患者发生复合心血管结局事件,安慰剂组4601例患者中有639例(13.9%)患者发生复合心血管结局事件(风险比为1.02;95%CI为0.92~1.14;97.5%CI单侧上限为1.14;绝对差位0.3个百分点;95%CI为−1.1至1.7;非劣效性单侧P=0.04)。
由此可见,在接受非心脏手术的患者中,氨甲环酸组的复合出血结局发生率显著低于安慰剂组。虽然复合心血管结局的组间差异很小,但氨甲环酸的非劣效性尚未明确。
原始出处:
P.J. Devereaux.et al.Tranexamic Acid in Patients Undergoing Noncardiac Surgery.NEJM.2022.https://www.nejm.org/doi/full/10.1056/NEJMoa2201171
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非心脏#
57
学习了
0
学习了
60
#非心脏手术#
0
#学习##期刊论坛#
77
不错的文章
62
NEJM上果然牛,感谢梅斯更新及时
52