Int J Cardiol:房颤一线治疗——导管消融 vs 药物治疗(MANTRA-PAF试验)
2015-09-12 MedSci MedSci原创
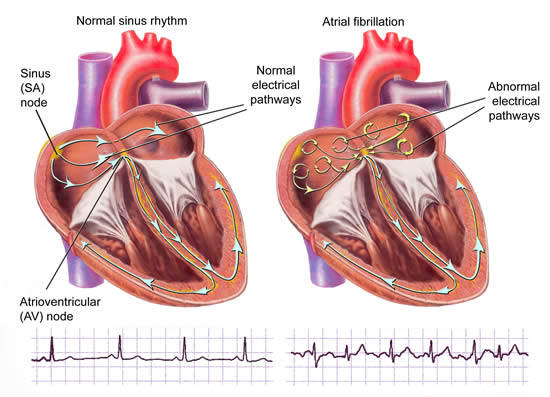
房颤是一种最常见的心律失常类型,该病可致患者生活质量下降并且与卒中及致残风险增加有关。房颤在老年患者中较为常见,其中60岁人群中发病率为2%,70岁以上人群中发病率达5%以上。Jens Cosedis Nielsen(丹麦奥尔胡斯大学医院)表示,多数临床医生在治疗症状性房颤时会选择抗心律失常药物治疗,而将导管消融作为药物治疗失败后的备用疗法,那么导管消融能否取代药物疗法治疗而作为一线治疗呢?这项结
房颤是一种最常见的心律失常类型,该病可致患者生活质量下降并且与卒中及致残风险增加有关。房颤在老年患者中较为常见,其中60岁人群中发病率为2%,70岁以上人群中发病率达5%以上。Jens Cosedis Nielsen(丹麦奥尔胡斯大学医院)表示,多数临床医生在治疗症状性房颤时会选择抗心律失常药物治疗,而将导管消融作为药物治疗失败后的备用疗法,那么导管消融能否取代药物疗法治疗而作为一线治疗呢?这项结果在ESC 2015上公布,并在Int J Cardiol上同步发表。
国际多中心试验MANTRA-PAF纳入了294例症状明显的房颤患者,随机选择导管消融或药物治疗作为受试者的一线治疗方法。2年结果显示,两种治疗方法均有效减少了受试者房颤发生,但均未体现出相对的优越性。
MANTRA-PAF研究者近期在ESC会上呈现了其5年随访结果,主要终点是心电图记录的7天内房颤负担,次要终点2年后症状性房颤负担、生活质量(SF-36调查问卷)及需要额外导管消融。
共245/294例患者完成了5年随访,其中125例接受了导管消融治疗,120例接受了药物治疗,研究者共收集到227例患者的心电图数据。结果显示,导管消融组未发生房颤(126/146 vs. 105/148,p=0.001)及症状性房颤(137/146 vs. 126/148, p=0.015)的患者多于药物治疗组,而且导管消融组房颤负担明显较低(房颤:p=0.003,症状性房颤:p=0.02),排除心电图数据缺失的影响后随访结果相似。Nielsen认为,这表明了导管消融作为一线治疗优于药物疗法,2年结果与5年结果不同的原因可能是两种疗法的作用机制存在差异。
2年时两组患者中需额外导管消融的数量不存在差异,5年时两组患者生活质量评分也无差异(身体评分p=0.88,精神评分p=0.94),但较基线时均有所改善,且与2年结果相同,这表明无论是通过导管消融还是药物治疗控制心律均可提高患者生活质量。
Nielsen总结道,导管消融作为一线治疗抑制阵发性房颤的效果优于药物治疗,医生在选择一线治疗策略时还须考虑患者的疾病负担与不同治疗策略的相关风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TRA#
87
#Cardiol#
103
#导管消融#
91
#消融#
88