Biology of Sex Differences:DHA补充剂或可抵消孕妇因压力对胎儿产生的不良影响
2021-03-25 MedSci原创 MedSci原创
在孕期时,饮食和环境对宝宝的健康至关重要,不仅会影响胎儿的出生体重,还会影响胎儿的大脑发育。流行病学研究表明,妊娠初期的缺氧,产前压力和营养不良,预示男性精神分裂症的风险增加,而在妊娠中期,产前压力可
在孕期时,饮食和环境对宝宝的健康至关重要,不仅会影响胎儿的出生体重,还会影响胎儿的大脑发育。流行病学研究表明,妊娠初期的缺氧,产前压力和营养不良,预示男性精神分裂症的风险增加,而在妊娠中期,产前压力可增加男性自闭症谱系障碍的患病率。

近日,发表在Biology of Sex Differences杂志上的一项研究显示,妊娠期补充二十二碳六烯酸(DHA)可预防因压力而给胎儿带来的早期发育的影响。

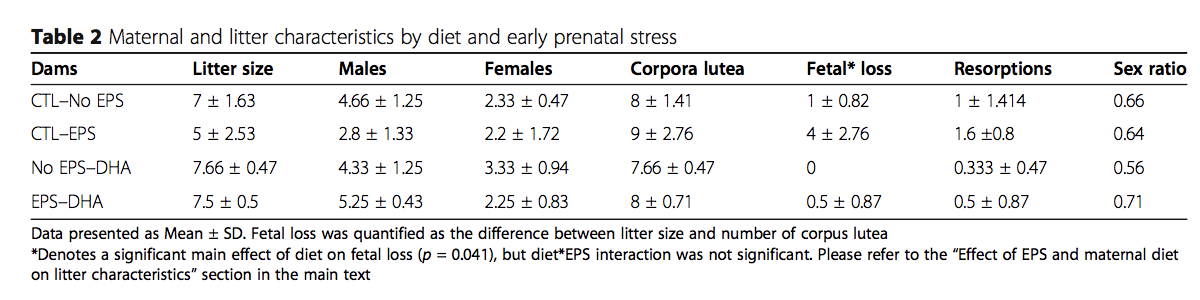
在这项研究中,研究人员将40只小鼠分为4组,第1组的母亲接受标准饮食,没有受到任何早期的产前压力(EPS)。第2组在暴露于EPS的同时获得标准饮食,包括节制,光线,噪音和掠食性动物威胁。第3组的饮食经补充DHA改良,但未暴露于EPS。第4组接受DHA补充和EPS。
结果发现,暴露于早期产前应激(EPS)的男性(但不包括女性)可降低胎盘和胚胎重量,但DHA的补充逆转了EPS导致胎盘和胚胎重量的下降。
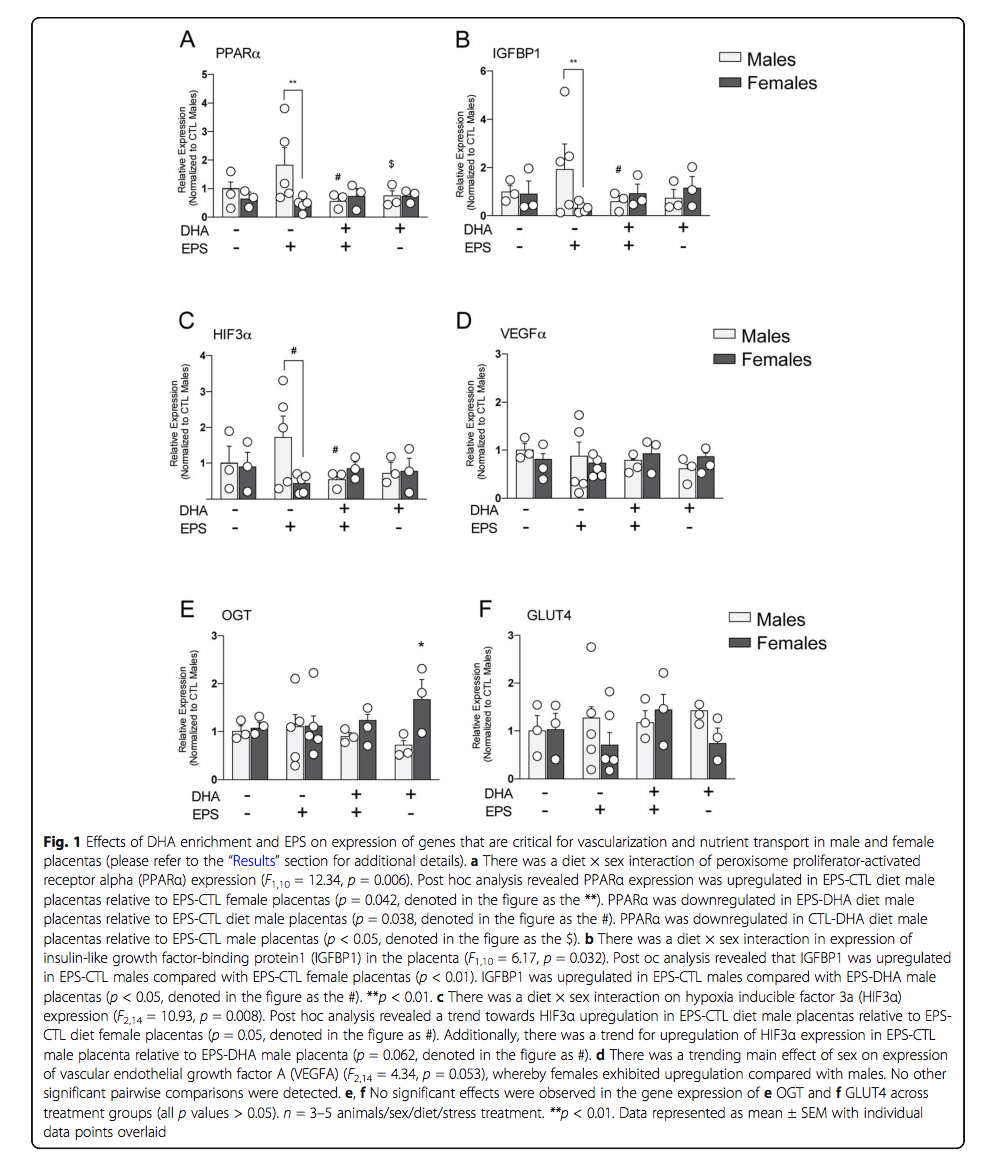
研究进一步发现,妊娠第一周母亲的压力似乎会影响胎盘的基因表达模式,而后代的性别决定了胎盘破裂的程度。其次,在高压力时期,补充DHA可缓解部分依赖于胎盘基因表达的失调。
研究人员表示,“妊娠前三个月的男性和女性胚胎代谢需求差异,再加上男性和女性胎盘对环境因素反应的差异,会增加男性神经发育障碍的风险。”
“我们仍需要进一步研究,以更好地了解将孕期,饮食对胎盘基因表达和后代健康的关联。”研究人员强调到。
原始出处
Eldin Jašarević et al, Maternal DHA supplementation influences sex-specific disruption of placental gene expression following early prenatal stress, Biology of Sex Differences (2021). DOI: 10.1186/s13293-020-00356-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Bio#
78
#Biol#
86
#Difference#
79
#Differ#
115
认真学习了
118