胸闷气短本以为心脏病 没承想竟是
2018-05-18 熊长明 肺血管病
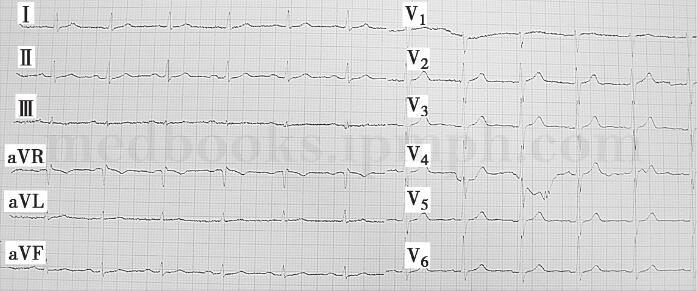
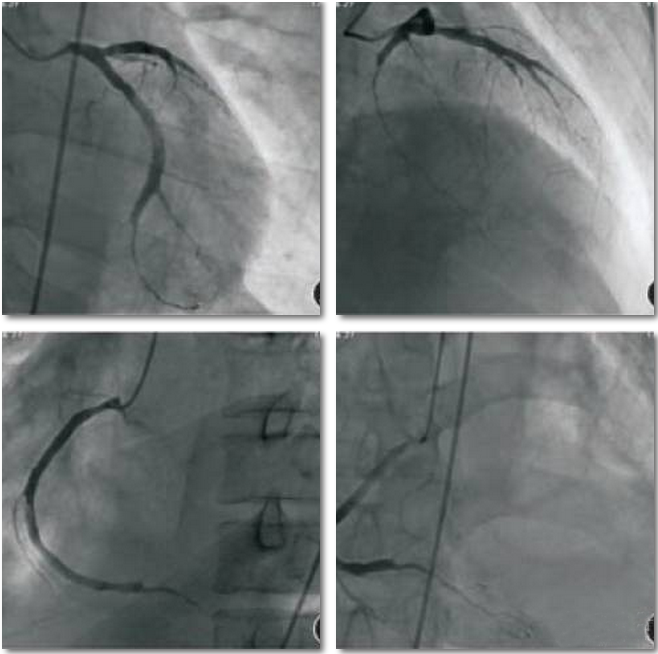
40岁男性患者,因间断低热2年,活动后气短、胸闷入院。患者自发病以来,体重明显下降,食欲缺乏。入院诊断:1.先心病,肺动脉狭窄?2.感染性心内膜炎。行超高速CT显示,前纵隔占位性病变,侵及主肺动脉及左右肺动脉,致肺动脉管腔狭窄,右心室增大。本例患者曾被误诊为先心病、肺动脉瓣上狭窄以及肺栓塞等疾病。患者到底所患何病?请阅读以下病例。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










感谢分享.
104
#胸闷#
75
#气短#
64
了解一下
103