Thorax:急性呼吸窘迫综合征患者不同生物学表型的聚类分析!
2017-04-28 xing.T MedSci原创
ARDS患者可分为两种生物学表型,其病死率有所不同,并且这四种生物标志物可准确地预测表型。
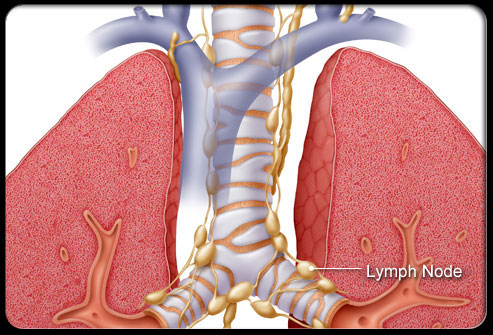
近日,胸部疾病领域权威杂志Thorax上发表了一篇研究文章,研究人员假设急性呼吸窘迫综合征(ARDS)患者可以根据于血浆中生物标志物的浓度进行分群,从而确定生物表型与死亡率之间的相关性。
在这项前瞻性观察性队列研究中,研究人员纳入了连续就诊的ARDS患者。在训练队列中,对炎症、凝血和内皮活化的20个生物标志物进行聚类分析提供了生物表型,不考虑任何结局数据。采用Logistic回归与逆向选择来选择预测性能最好的生物学标志物,在另一个单独的队列中,人员对这些预测的表型进行了验证。多变量Logistic回归分析被用来定量与死亡的独立相关性。
两种表型纳入了454例患者,这两组表型分别命名为非炎性表型(n=218)和炎性表型(n=236)。在训练队列中,选择的四个生物标志物(白细胞介素6、干扰素-γ、血管生成素1/2和纤溶酶原激活物抑制剂-1)可以用来准确地预测表型(接受者操作特征曲线下面积为0.98,95%可信区间为0.97-0.99)。在训练队列中,死亡率为分别为15.6%和36.4%(P<0.001),在验证队列(n=207)中,死亡率为分别为13.6%和37.5%(P<0.001)。炎性表型独立于混杂因素与ICU死亡率相关(训练队列比值比为1.13,95%可信区间为1.04-1.23;验证队列比值比为1.18,95%可信区间为1.06-1.31)。
ARDS患者可分为两种生物学表型,其病死率有所不同,并且这四种生物标志物可准确地预测表型。
原始出处:
L D Bos, et al. Identification and validation of distinct biological phenotypes in patients with acute respiratory distress syndrome by cluster analysis.Thorax. 2017. http://dx.doi.org/10.1136/thoraxjnl-2016-209719
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习并分享了
80
#综合征#
71
#表型#
65
#呼吸窘迫#
73
#生物学#
82
学习啦谢谢分享
108