喜大普奔!BRAF突变的黑色素瘤患者生存希望增加!
2015-11-13 QQduhq 译 MedSci原创
FDA批准,可将cobimetinib和vemurafenib联合使用,用于治疗转移和扩散且不能用手术切除的黑色素瘤患者或含有突变BRAF基因的肿瘤患者。
FDA批准,可将cobimetinib和vemurafenib联合使用,用于治疗转移和扩散且不能用手术切除的黑色素瘤患者或含有突变BRAF基因的肿瘤患者。Genentech公司研发Vemurafenib(通用名Zelboraf)和cobimetinib联合使用以治疗黑色素瘤。
如果黑色素瘤患者没有得到早期诊断,它可能会蔓延到身体的其他部位,即出现转移。约一半的转移性黑色素瘤患者有突变BRAF基因。
导致黑色素瘤出现的变异基因有两种形式——BRAF V600E和BRAF V600K,这些可以通过一项经FDA批准的测试检验出来。FDA建议,医生应该在开具药物处方前对病人进行肿瘤标记物筛查以查看他们是否有突变基因。
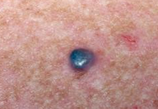
皮肤癌是美国最常见的癌症。大部分皮肤癌是由于民众经常暴露于紫外线(UV)导致的。黑素瘤患者占所有皮肤癌患者的1/50,但是会导致大多数患者的死亡。黑色素细胞瘤可由表皮黑色素细胞,痣细胞或真皮成黑色素细胞组成。美国国家癌症研究所估计,在2015年,美国近74000人罹患黑素瘤,近10000人将死于这种疾病。
FDA的Richard Pazdur博士认为,FDA批准两种药物联合使用用于治疗黑色素瘤很有针对性。Vemurafenib单独使用不能完全抑制含有BRAF基因的黑色素瘤患者的肿瘤细胞,使肿瘤继续增长。Cobimetinib药物可通过阻断一种被称为MEK的酶的活动,起到抑制肿瘤细胞生长的作用。
结果表明,平均而言,服用vemurafenib和cobimetinib两种药物的患者(实验组)肿瘤转移和症状恶化时间出现较晚,平均12.3月后出现肿瘤转移;相比之下,服用vemurafenib +安慰剂的对照组患者肿瘤转移症状出现较早,时长约7.2个月。此外,实验组患者的寿命更长,17月后约65%的患者存活;相比之下,对照组仅有一半的人存活。药物使用不同,对肿瘤也有不同的影响:接受药物组合的实验组患者中,约70%患者的瘤体缩小,是对照组的2倍。
联合治疗最常见的副作用是腹泻、对紫外线的敏感性、恶心、发烧和呕吐。
这项研究对含有BRAF突变基因的黑色素瘤患者而言是福音,不仅可减轻症状,也可缩小肿瘤,同时出现的药物副作用更少。
原始出处:
Drug combination for advanced melanoma wins FDA approval,MNT,12,Nov,2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者生存#
80
#色素#
70
#BRAF#
95
#BRAF突变#
85
#黑色素#
69
#黑色素#
62
。
174