无创新疗法治疗震颤取得里程碑进展,“磁波刀”神外解决方案获批药监局批准在华正式投入临床
2021-05-24 Oranhgy MedSci原创
5月21日,由中华医学会、中华医学会神经外科学分会主办,上海医学会神经外科分会承办,复旦大学附属华山医院协办的“中华医学会神经外科学分会第十九次学术会议”在上海召开。
5月21日,由中华医学会、中华医学会神经外科学分会主办,上海医学会神经外科分会承办,复旦大学附属华山医院协办的“中华医学会神经外科学分会第十九次学术会议”在上海召开。本次大会以“数字化时代的神经外科”为主题。
会议召开之际,Insightec医视特公司于5月22日在受邀参加中华医学会第十九次全国神经外科学术大会期间举行了其神经外科解决方案磁共振引导聚焦超声脑部系统(Exablate® Neuro)的中国上市会,向业界与公众宣布该方案将正式投入临床,用以治疗药物难治性特发性震颤(essential tremor,ET)或以震颤为主型帕金森病(Parkinson's disease,PD)。
磁共振引导聚焦超声脑部系统上市启动仪式。从左至右:木场雄一郎先生、李勇杰教授、高国栋教授、余新光教授、邱鹏先生
Insightec医视特磁共振引导聚焦超声脑部系统(Exablate® Neuro)于2021年初获得中国国家药品监督管理局的上市批准,此前在2016年获得美国FDA批准,2012年获得欧洲CE认证。该技术也被称为“磁波刀”,为患者提供了一种无创、磁共振成像引导的丘脑手术。治疗过程无需开刀、钻孔或开颅手术,无植入物。单次疗程后,震颤即能得到缓解,且副作用极小,可以当天回家。
众所周知,帕金森病是一种常见的神经系统变性疾病,老年人多见,平均发病年龄为60岁左右。起病隐袭,进展缓慢。震颤是帕金森病给患者带来的主要症状之一。首发症状通常是一侧肢体的震颤或活动笨拙,进而累及对侧肢体。临床上主要表现为静止性震颤、运动迟缓、肌强直和姿势步态障碍。约70%的患者以震颤为首发症状,多始于一侧上肢远端,静止时出现或明显,随意运动时减轻或停止,精神紧张时加剧,入睡后消失。手部静止性震颤在行走时加重。
根据帕金森病基金会的估计,2016年,全球有超过1000万患者,其中美国有100多万。在中国,帕金森病患病率在几十年中从76/10万增加到100/10万。目前中国有超过300万帕金森病人,65岁以上中老年人发病率为1.7%,占全球患者总数的三分之一。预计到2030年,患病人数将达到近500万人,几乎占到全球帕金森病患病人数的一半。
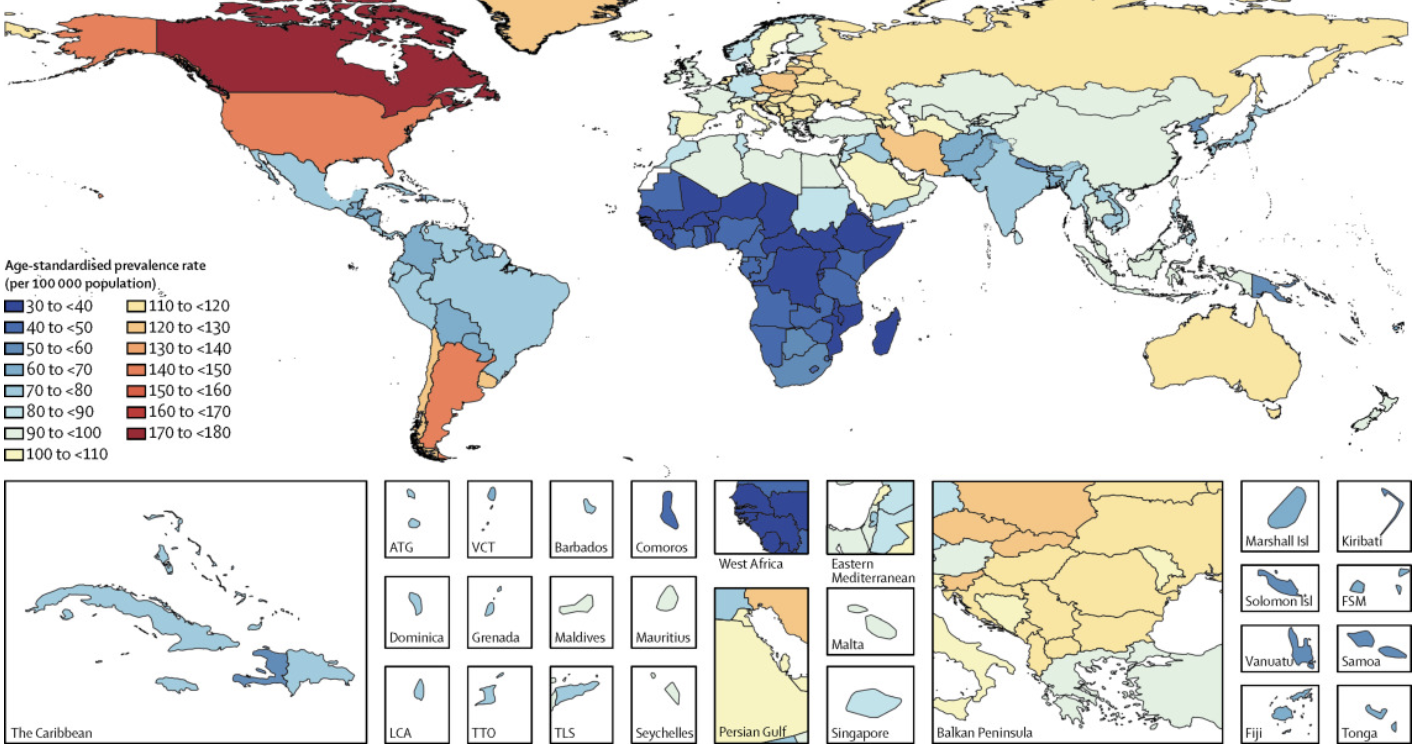
2016年,全球帕金森患病率Global, regional, and national burden of Parkinson's disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. DOI:https://doi.org/10.1016/S1474-4422(18)30295-3
特发性震颤(essential tremor, ET)是是最常见的运动障碍病。其中,以手部抖动为明显特征的震颤会使患者在生活、学习、工作中无法完成精细的动作,严重者甚至生活无法自理。根据中华医学会神经病学分会帕金森病及运动障碍学组和中国医师协会神经内科医师分会帕金森病及运动障碍学组制定的《中国原发性震颤的诊断和治疗指南(2020)》,该病在人群中的患病率约为0.9%,并随着年龄的增长而升高,65岁以上老年人群的患病率约为4.6%。
北京功能神经外科研究所创所所长、首都医科大学宣武医院功能神经外科创科主任、香港大学深圳医院神经医学中心主任高级顾问医生李勇杰教授在接受梅斯医学采访时表示,“对于患有特发性震颤,震颤为主型的帕金森病的患者,传统治疗方法为药物治疗和手术治疗。但现如今很多这类患者患者面临药物难治的问题。为改善震颤症状给患者带来的严重影响,提高患者生活自理能力,手术治疗就成了一个必要的选项。以往的神经外科功能手术,需要开刀或钻颅手术,有些还要在体内植入设备,限制了某些不愿手术、或年龄不适合手术的患者进行治疗。”

李勇杰教授、潘隆盛教授、邱鹏先生、木场雄一郎先生接受媒体采访
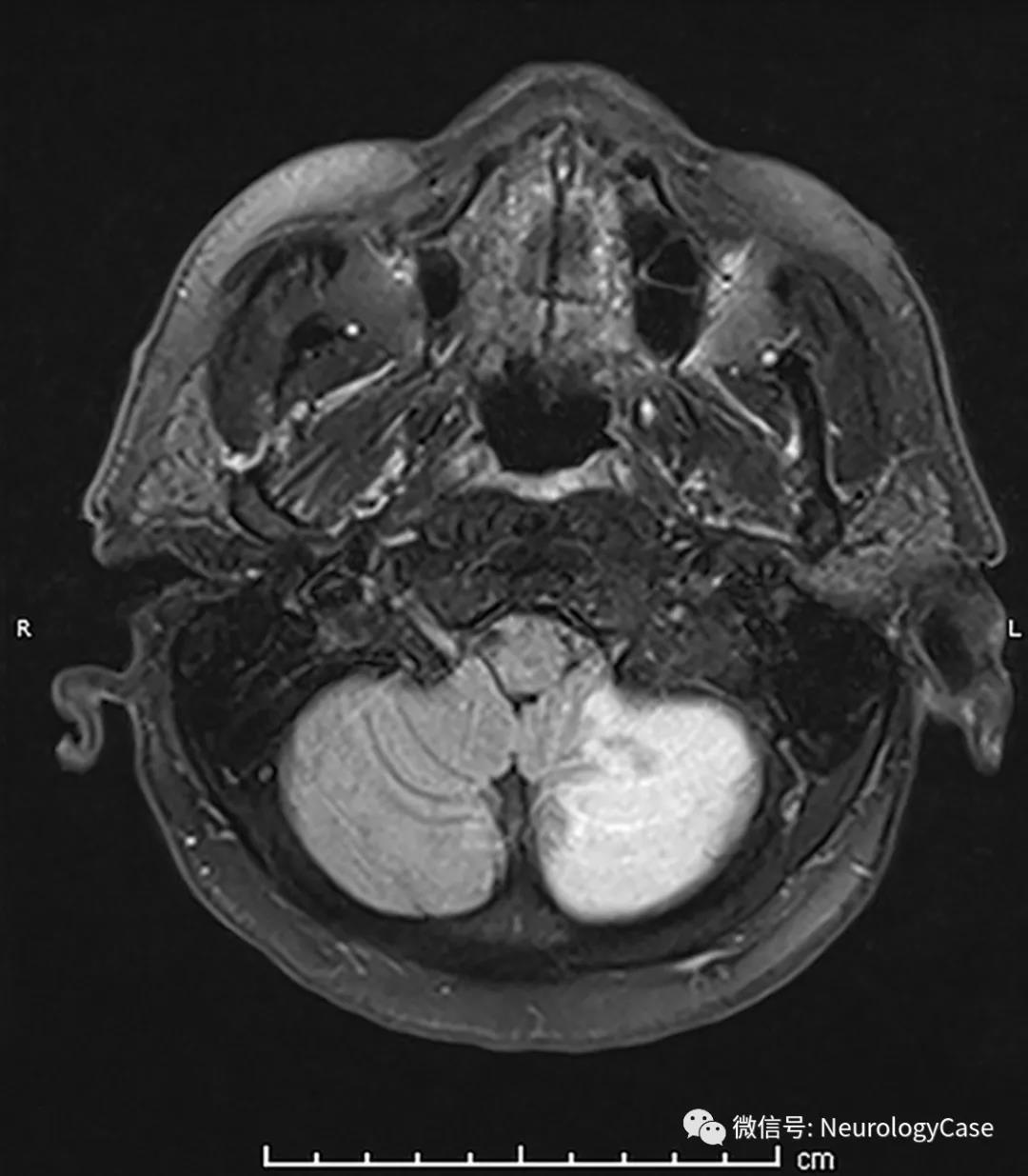
Insightec医视特中国总经理邱鹏先生向梅斯医学介绍道,高强度聚焦超声的研究始于一九四零年代,最早就是希望做颅内治疗,但因为声波很难穿透颅骨,直到现在相控阵技术结合磁共振的发展,解决了这一难题。现在的“磁波刀”技术可以不用开颅,直接通过声波进行颅内治疗。患者戴上有1024个超声发射束的聚焦超声头盔,调整声波相位,同时聚焦到颅内一点进行消融,达到治疗目的。
同时,解放军总医院是中国大陆地区首家使用“磁波刀”治疗震颤的医院。解放军总医院“磁波刀”治疗系统项目负责人、解放军总医院第一医学中心神经外科医学部主任医师教授潘隆盛向梅斯医学介绍道,“‘磁波刀’治疗过程中,按照MRI 标准立体定向治疗计划标定、图像融合、靶点确认、初始剂量的温度校正、实验性升温的治疗温度验证、患者生理反馈进行治疗靶区的精准定位及最终的确定性剂量毁损消融。治疗过程中经历物理校正、电子校正、临床验证、影像验证等多重确认,这些步骤可有效保证治疗的效果和安全性。尤其是术中治疗过程中,在MRI温度序列监测下,可以实时获得靶点温度值,从而保证治疗过程的安全。”
事实上“磁波刀”在国外已有很多相关研究。此前,发表在NEJM上的研究表明,MRI引导下的聚焦超声丘脑切开术减少了原发性震颤患者的手部震颤。
A Randomized Trial of Focused Ultrasound Thalamotomy for Essential Tremor. DOI: 10.1056/NEJMoa1600159
研究人员招募了76名对至少两次药物治疗没有反应的中重度本质性震颤患者,以3:1的比例随机分配他们接受单侧聚焦超声丘脑切除术(实验组)或无手术(对照组)。在基线和1、3、6和12个月时进行震颤临床评定量表和基本震颤生活质量调查表的管理。震颤评估由独立的神经学家小组进行录像和评分。主要结果是手震颤从基线到3个月的变化的组间差异,用32分制评分(分数越高表示震颤越严重)。3个月后,假手术组的患者可以转为主动治疗。
研究结果显示,与对照组(从16.0分到15.8分)相比,实验组术后的手部颤动评分改善更多(从基线的18.1分到3个月的9.6分);组间平均变化差异为8.3分(95%置信区间[CI],5.9到10.7;P<0.001)。实验组的改善在12个月时保持不变(从基线的变化,7.2分;95%CI,6.1至8.3)。同时发现,实验组评估残疾和生活质量的次要结果措施也有改善(两个比较的P<0.001)。
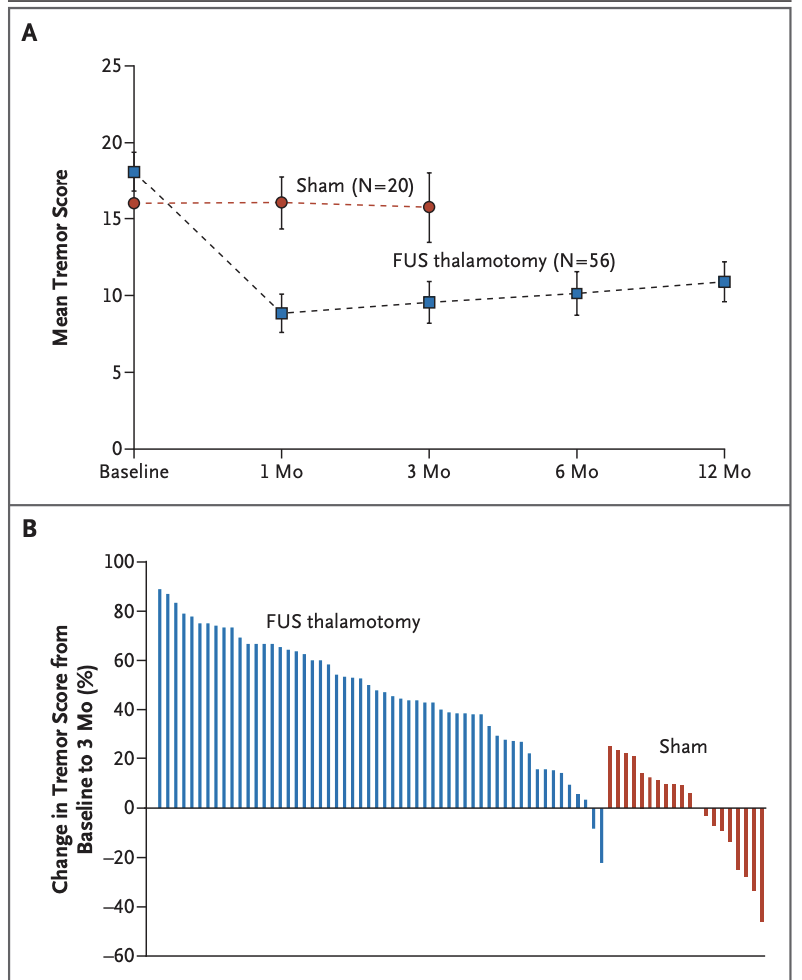
震颤分数
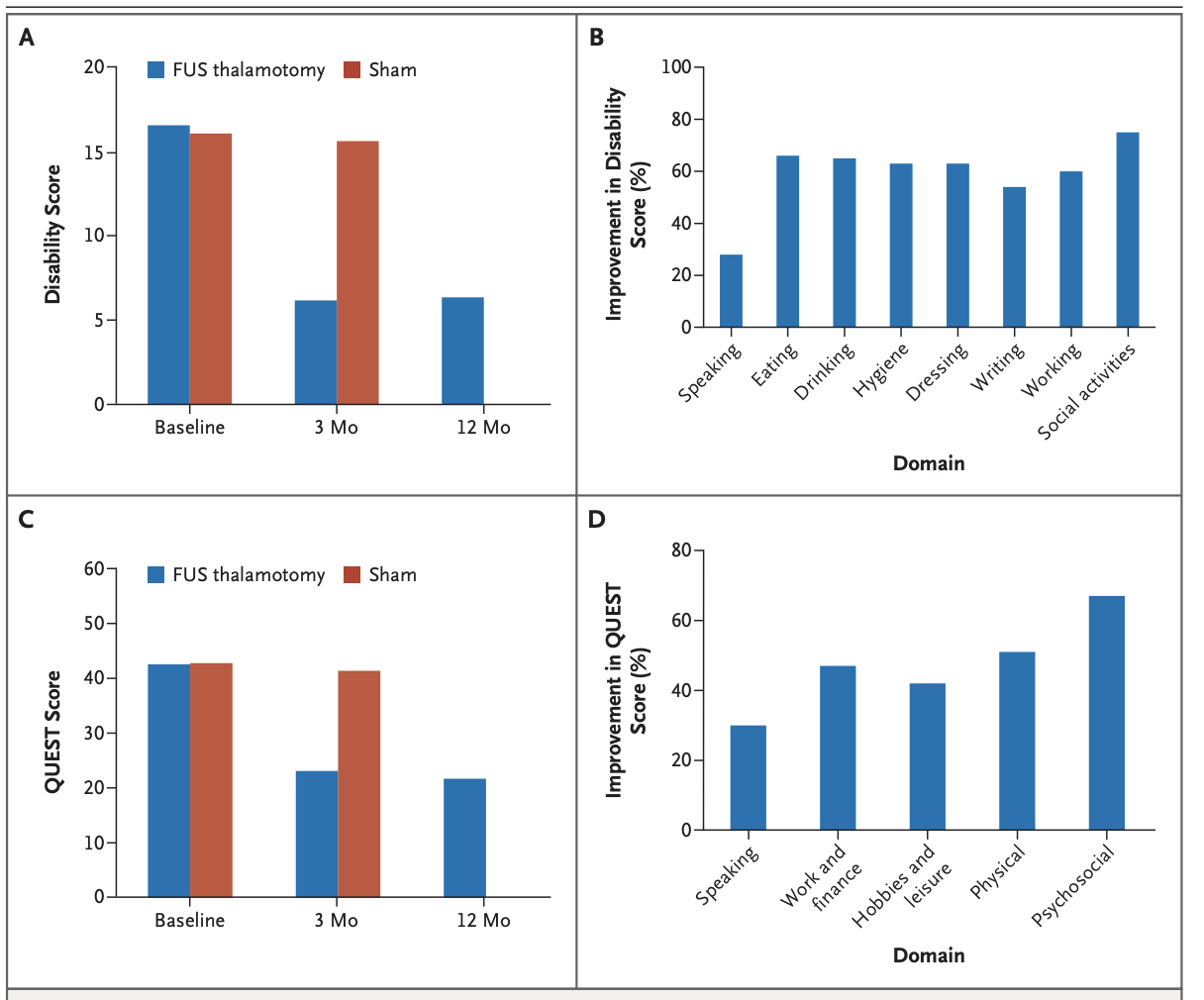
日程生活的功能性活动以及生活质量
该研究表明磁波刀减少了原发性震颤患者的手部震颤的同时,也改善了患者生活质量。
目前,专家还在探索“磁波刀”技术的更多适应症,未来的临床应用将更为广泛。解放军总医院神经外科医学部神经外科研究所所长、中国医师协会神经外科医师分会副会长余新光介绍,帕金森病、特发性震颤、阿尔海默氏病、强迫症、抑郁症、自闭症等大量脑功能疾病,严重困扰人类健康。总医院神经外科团队聚焦“脑科学”,致力新型脑功能疾病治疗研究。 “磁波刀”治疗精准性、无创性、可开放血脑屏障等优势,也为脑功能疾病、脑肿瘤疾病等传统治疗非常棘手的疾病,提供了新的治疗选择和新的技术手段。”
自问世以来,Insightec医视特的磁共振引导聚焦超声脑部系统(Exablate® Neuro)得到了业界广泛肯定,获得了包括有医疗器械“诺贝尔奖”之称的盖伦奖(Annul Prix Galien)2017最佳医疗科技产品奖、创新界的“奥斯卡”爱迪生奖(Edison Award)2018最佳医疗创新奖等多个奖项。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#里程碑#
121
#解决方案#
81
#创新#
75
#药监局#
112
#震颤#
145
#新疗法#
81