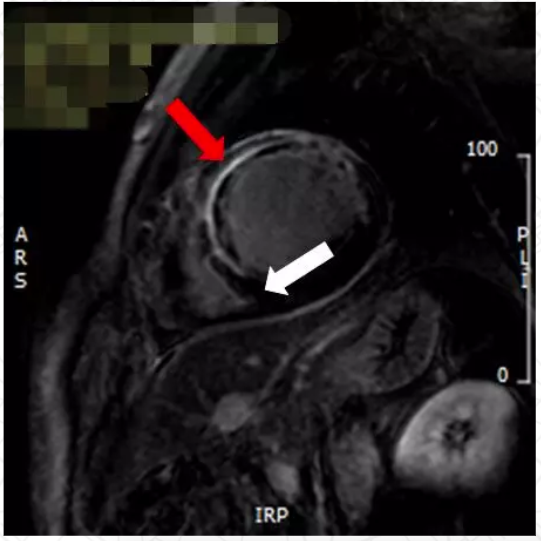
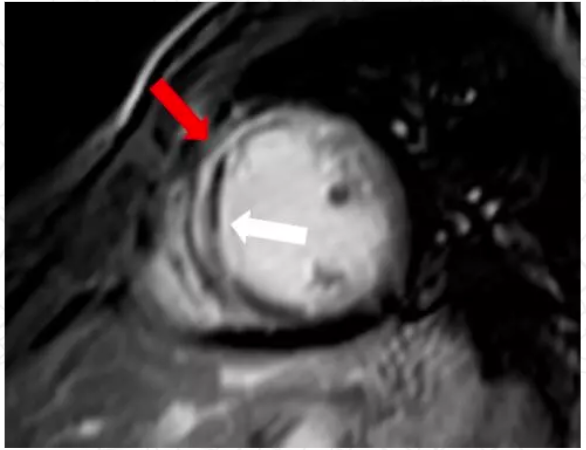
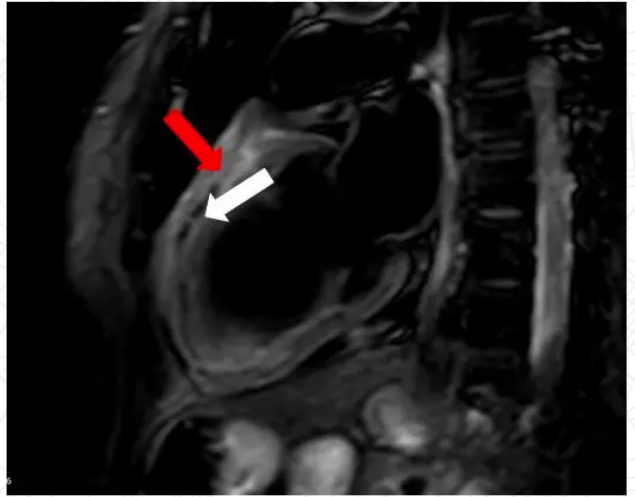
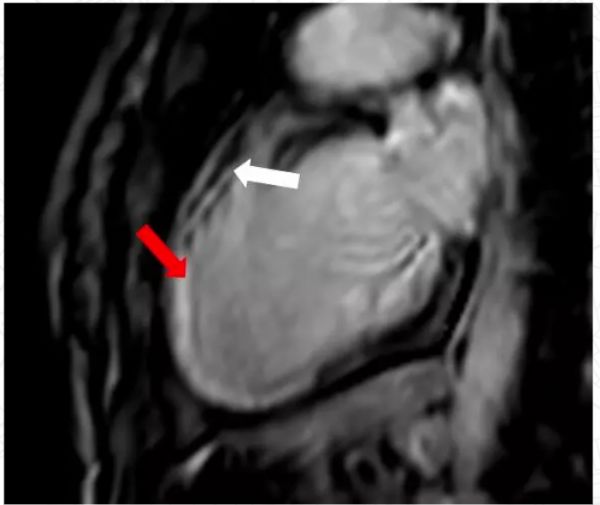
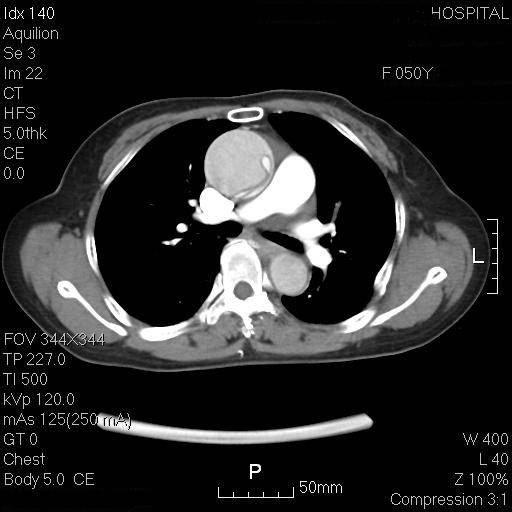
急性心梗要不要做核磁检查?浅谈心脏磁共振在急性ST段抬高型心肌梗死评价中的作用
2018-02-12 葛恒 中国医学论坛报今日循环
急性ST段抬高型心肌梗死(STEMI)是导致心源性死亡的重要原因。尽管广泛应用的再灌注治疗可紧急恢复闭塞冠脉的血流,挽救部分濒死心肌并降低急性期死亡率,但存活患者仍可能因大量丢失心肌而出现心力衰竭,导致各类心血管事件

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















学习一下谢谢
80
#急性心梗#
71
#磁共振#
61
#心脏磁共振#
73
#ST段抬高#
0
#评价#
65
#ST段#
57
学习一下谢谢
90
∵学习了.谢谢分享.
88