PNAS:可用于心脏再生的创新性“工具”
2016-08-14 佚名 生物谷Bioon.com
图片来源:medicalxpress.com 心血管疾病是引发美国人群死亡的主要原因,每年都有四分之一的人死于心血管疾病,而且患者心脏病发作后5年的生存率不如大多数癌症,目前患者遭遇的最大问题就是其机体并不能进行有效的损伤后修复,近日来自休斯顿大学的研究者通过研究在此领域获得了巨大进展。研究者开发了一种新型策略来帮助患者进行心脏肌肉的再生,相关研究刊登于国际杂志PNAS上。 人类的心脏是一
图片来源:medicalxpress.com
心血管疾病是引发美国人群死亡的主要原因,每年都有四分之一的人死于心血管疾病,而且患者心脏病发作后5年的生存率不如大多数癌症,目前患者遭遇的最大问题就是其机体并不能进行有效的损伤后修复,近日来自休斯顿大学的研究者通过研究在此领域获得了巨大进展。研究者开发了一种新型策略来帮助患者进行心脏肌肉的再生,相关研究刊登于国际杂志PNAS上。
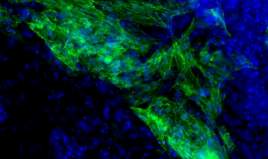
人类的心脏是一种并不能进行再生的器官,而且心肌细胞的数量会随着年龄增长而不断下降,在损伤期间细胞就会流失,比如心脏病发作等,损伤的细胞通常会被结缔组织移除,这称之为纤维化过程,该过程会导致心脏泵血功能的却是,而这就是心脏疾病同癌症一样死亡率较高的主要原因。
为了找到一种解决方法,研究者Liu和其同事对胚胎中心脏形成的机制进行了研究,他们非常好奇他们所发现的新型调节子是否能够将人类的成纤维细胞转化为心脏肌肉细胞。研究者Schwartz说道,我们首次通过研究来将人类的成纤维细胞转化为心肌细胞,而且我们希望这些microRNA调节子应该具有潜在的活性。
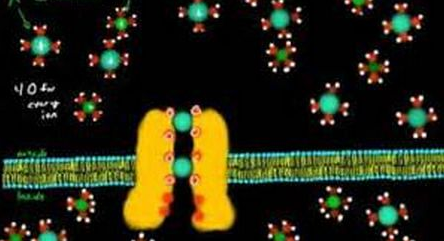
在美国航天局进行的一项空间站实验中,研究者Schwartz就通过研究揭示了空间站中特殊的环境如何将机体成纤维细胞成功转化为心脏肌肉细胞,而microRNA调节子在这一过程中就起到了实质性的帮助作用。microRNA曾经一度被认为是“遗传垃圾”,其在基因调节过程中扮演着重要的角色。文章中,利用小鼠遗传工具,研究者就在培养皿中追踪了小鼠心脏肌肉形成的关键过程,这项研究工作包括很多步,最重要的是,研究者首先在心脏的早期祖先细胞中鉴别出了大约140个microRNA分子,随后研究者对这些microRNA进行筛选来寻找可以驱动心肌细胞形成的关键microRNA分子,最后研究者发现了关键的miR-322/503簇分子。
最后研究者希望通过后期更为深入的研究,利用这些筛选出的microRNA分子来治疗人类心脏病发作以及心力衰竭等心血管疾病,当然研究人员还将开发出多种小鼠模型来进行更为深入的探索。
Xiaopeng Shena, Benjamin Soibama,b, Ashley Benhama,b, Xueping Xuc, Mani Chopraa, Xiaoping Penga, Wei Yua, Wenjing Baoa, Rui Lianga, Alon Azaresb, Peijun Liud, Preethi H. Gunaratnea, Mark Mercolae, Austin J. Cooneyc, Robert J. Schwartza,b, and Yu Liua,1.miR-322/-503 cluster is expressed in the earliest cardiac progenitor cells and drives cardiomyocyte specification.PNAS doi:10.1073/pnas.1608256113
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PNAS#
74
文章很好值得关注
129
长见识了
124
新技术,谢谢
108
值得学习
112
值得学习
126
继续学习
90
继续关注
59
#创新#
75