Ann Vasc Surg:AIA或CIAA血管内修复术中IBSG植入系统是IIA保存安全且有效的技术
2020-11-13 MedSci原创 MedSci原创
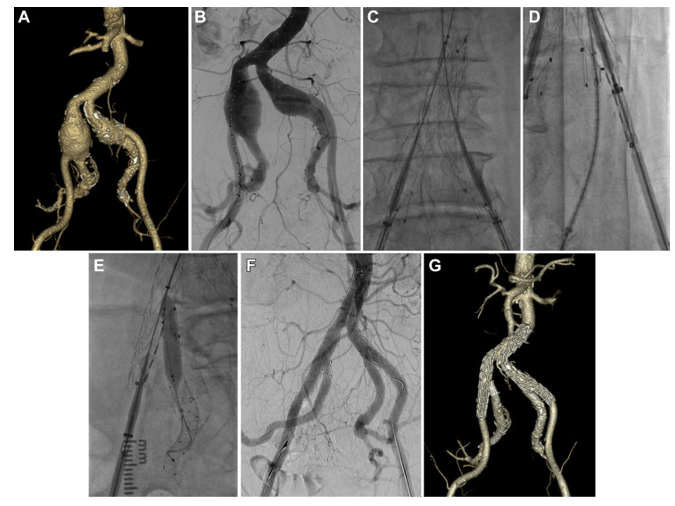
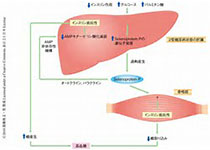
牺牲髂内动脉(IIA)可能会导致主动脉髂动脉瘤(AIA)或髂总动脉瘤(CIAA)血管内修复后缺血。本研究旨在评估一种新型髂动脉分叉支架移植(IBSG;Lifetech Scientific,中国深圳)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#修复术#
74
#ASC#
68
#IBS#
74
#植入#
75
学习了
102