生物信息学分析揭示了肺动脉高压的标志基因和潜在的治疗靶点
2021-11-15 刘少飞 MedSci原创
肺动脉高压(PAH)是一种罕见的心血管疾病,死亡率非常高。目前可用的治疗策略可以改善症状,但不能从根本上逆转病情。CDC5L和DDX46可能是 PAH 的标记基因和潜在的治疗靶点。
肺动脉高压(PAH)是一种由多种因素引起的罕见的致命疾病。它的特点是血管增厚和血管阻塞性重塑,导致肺血管血压升高,最终导致右心室心力衰竭,甚至死亡。根据之前的研究,每 100 万人中有 15 人患有肺动脉高压。目前针对促血管和增生介质的疗法,例如磷酸二酯酶 5 (PDE-5) 抑制剂、内皮素受体拮抗剂 (ERA) 和前列环素受体激动剂,可改善活动耐力和增强心脏功能。然而,上述药物不能针对肺血管重构和炎症等其他 PAH 病因,肺动脉高压仍然是一种无法治愈的心肺疾病。目前,PAH 仍然无法治愈。因此,阐明PAH的基因表达谱有助于探索PAH的发病机制或寻找潜在的治疗方法。
快速发展的系统生物学分析已成为预测疾病相关基因、疾病亚型和疾病治疗的有力工具。加权基因共表达网络分析 (WGCNA) 广泛用于研究微阵列样本。通过计算基因之间的相关性,WGCNA 可以将具有相似表达模式的基因集合(模块)聚类,分析模块与样本特征之间的关联,映射每个模块中的网络并识别枢纽基因。自出版以来,WGCNA 已被用于许多生物和医学科学领域,例如癌症和小鼠遗传学.
在这项研究中,我们对数据集构建了一个相关网络。还进行了京都基因百科全书 (KEGG) 和基因本体论 (GO) 分析以研究潜在机制。在关键模块中发现CDC5L和DDX46,然后通过其他数据集和接收器操作特征 (ROC) 曲线进行评估。随后,在 PAH 动物模型中使用定量逆转录聚合酶链反应 (qRT-PCR) 对这两个潜在的标记基因进行了双重确认。我们的研究可能会指出治疗 PAH 的潜在目标。
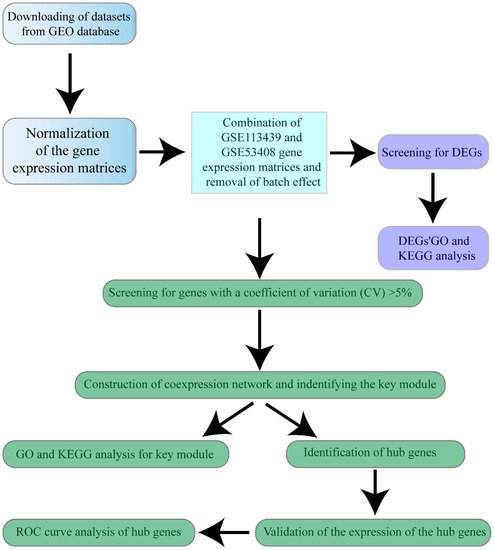
研究设计的工作流程:
研究发现:
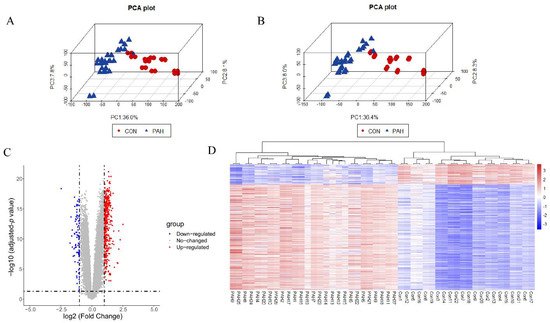
数据预处理和 DEGs 筛选
GSE113439 和 GSE53408 表达矩阵组合在一起,包含来自 27 名对照和 22 名 PAH 患者的肺样本。接下来,批次效应被消除,批次效应调整前后的样本分布在 3D PCA 图中说明(图下)。共鉴定出 542 个 DEG。火山图和 DEG 热图如下图C、D 所示。DEGs 的表达也表明了对照组和 PAH 组之间的差异。
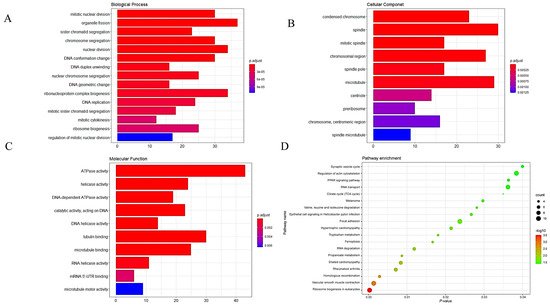
DEG 的 GO 和 KEGG 分析
在 GO 分析中,最丰富的生物过程 (BP) 术语与核糖体生物发生、有丝分裂核分裂的调节和有丝分裂胞质分裂相关。细胞成分 (CC) 最丰富的术语主要与前核糖体和中心粒有关。最丰富的分子功能 (MF) 术语与 DNA 依赖性 ATPase 活性和 DNA 解旋酶活性相关(下图A-C)。在 KEGG 分析中,DEG 在真核生物、黑色素瘤、肥厚型心肌病和扩张型心肌病的核糖体生物发生中富集(图D)。
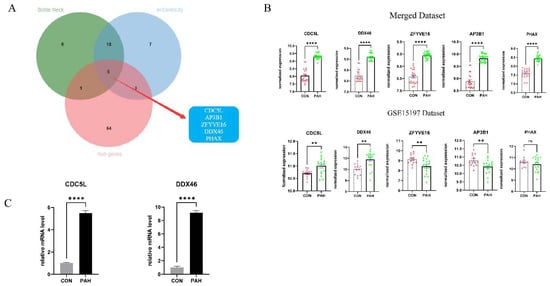
候选标记基因的验证
在数据集中,重叠的五个候选标记基因在 PAH 样本中显着上调(p值 < 0.001)。在验证数据集 GSE15197 中,我们发现多环芳烃样品中CDC5L和DDX46的表达显着上调。( p值 < 0.01)。(图B)。
我们观察到肉鸡也患有 PAH,可以作为探索 PAH 机制的优秀 PAH 模型。从一组独立的对照和 PAH 鸡的肺组织中提取 cDNA 样品。从 cDNA 样品获得的 qRT-PCR 结果表明,Cdc 5l和Ddx46在 PAH 组中均显着上调(p值 < 0.001)(图C)。
研究结论:
总之,通过整合和分析多个数据集,并通过WGCNA分析建立共表达网络,鉴定了PAH的两个潜在标记基因CDC5L和DDX46。通过 GO 和 KEGG 分析,核糖体生物合成、中心粒、ATPase 活性、解旋酶活性、肥厚型心肌病、黑色素瘤和扩张型心肌病通路可能与 PAH 相关。总之,我们的发现为了解 PAH 的发病机制提供了新的视角。
参考文献:
Li A, He J, Zhang Z, Jiang S, Gao Y, Pan Y, Wang H, Zhuang L. Integrated Bioinformatics Analysis Reveals Marker Genes and Potential Therapeutic Targets for Pulmonary Arterial Hypertension. Genes (Basel). 2021 Aug 28;12(9):1339. doi: 10.3390/genes12091339. PMID: 34573320; PMCID: PMC8467453.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#动脉高压#
67
#生物信息学分析#
98
#治疗靶点#
73
#生物信#
69
生信加验证性价比高高的
131
很好的启示
85