Heart:绝经后乳腺癌幸存者内分泌治疗与心血管风险
2020-11-15 MedSci原创 MedSci原创
与他莫昔芬使用者相比,AI使用者几项心血管结局较高风险似乎是由他莫昔芬的保护作用而不是AI的心脏毒性作用所驱动。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究旨在评估他莫昔芬和芳香酶抑制剂(AIs)对绝经后女性乳腺癌幸存者12种临床相关心血管结局风险的影响。
研究人员利用英国初级保健和医院数据(2002-2016年)和美国监测、流行病学和最终结果医疗保险数据(2008-2013年)对绝经后乳腺癌的女性进行了两项前瞻性队列研究,并使用Cox调整比例风险模型比较了AI和他莫昔芬使用者的心血管风险;在美国,研究人员还比较了两种药物都使用者和未接受内分泌治疗的女性。
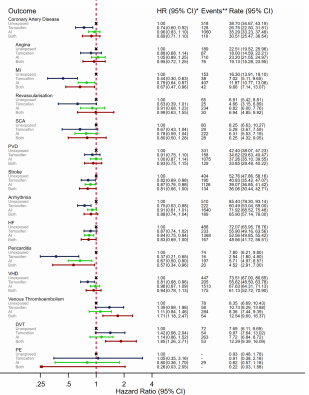
该研究纳入了10005名(英国)和22027名(美国)绝经后乳腺癌妇女。在这两个国家中,与他莫昔芬使用者相比,AI使用者冠状动脉疾病风险更高(英国年龄标准化的发病率:每1000人每年10.17 vs. 7.51;HR:1.29,95%CI为0.94至1.76;美国的年龄标准化的发病率:每1000人每年36.82 vs. 26.02,HR:1.29,95%CI为1.06至1.55)。但是,与未接受内分泌治疗的患者进行比较(美国数据)显示,任一药物使用著的风险并未升高,而他莫昔芬使用者的风险较低(他莫昔芬与未暴露人群相比,年龄标准化发病率:每1000人每年26.02 vs. 35.19,HR:0.74 ,95%CI为0.60至0.92;AI与未暴露人群相比,年龄标准化发病率:36.82 vs. 35.19,HR:0.96,95%CI为0.83至1.10)。其他心血管结局(心律不齐、心力衰竭和瓣膜性心脏病)的情况也相似。正如预期的那样,他莫昔芬使用者静脉血栓栓塞发生率高于AI使用者和未暴露者。
由此可见,与他莫昔芬使用者相比,AI使用者几项心血管结局较高风险似乎是由他莫昔芬的保护作用而不是AI的心脏毒性作用所驱动。
原始出处:
Anthony A Matthews.et al.Endocrine therapy use and cardiovascular risk in postmenopausal breast cancer survivors .heart.2020.https://creativecommons.org/licenses/by/4.0/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#分泌#
88
#血管风险#
59
#绝经#
66
#ART#
62
#HEART#
90
#绝经后#
82
感谢各位的分享!
110
心血管疾病会增加#乳腺癌#的死亡风险。
167
#乳腺癌#的治疗效果越来越好,现在大家关心的是这些患者的长期#心血管#风险了!这是当前热点
180
赞
123