ISC2018:全新AHA/ASA急性缺血性卒中指南为早期启动强化他汀治疗再添力荐
2018-01-27 国际循环编辑部 国际循环
备受关注的2018 AHA/ASA急性缺血性卒中早期管理指南(以下简称新指南),在大会第一天重磅发布,作为全球缺血性卒中管理指南的风向标,新指南将对急性缺血性卒中管理带来哪些影响?
2018年1月24~26日,一年一届全球卒中盛会——国际卒中大会(International Stroke Conference,ISC)于美国洛杉矶隆重召开。备受关注的2018 AHA/ASA急性缺血性卒中早期管理指南(以下简称新指南),在大会第一天重磅发布,作为全球缺血性卒中管理指南的风向标,新指南将对急性缺血性卒中管理带来哪些影响?
新指南改变了以往指南大段文字描述的方式,采用简洁明快的表格,使人一目了然,具有很强的落地指导性。新指南在急性缺血性卒中院前处理、急诊评估、静脉溶栓、血管内治疗和院内管理等方面做了较大程度的更新,在180项推荐意见中,有50项改写的推荐意见及61项新的推荐意见。
血管内治疗是指南更新的热点之一,与大家预料的一样,根据最新重磅研究DAWN和DEFUSE-3,进行了超时间窗更新。从静脉溶栓3~4.5小时时间窗,血管内治疗6小时时间窗到如今血管内治疗24小时时间窗。我们看到的不是盲目地扩大时间窗,而是基于多种影像筛选模式挑选最合适的患者。
我们注意到与2013年指南相比,新指南对他汀类药物在院内治疗的应用推荐做了显著更新:2013年指南仅把他汀作为神经保护剂进行推荐,新指南则不再局限于他汀的神经保护剂范畴,而是将其作为院内治疗的重要部分,强调他汀在急性缺血性卒中患者中的治疗作用。
在具体谈到他汀治疗推荐之前,有必要先说一说新指南中针对二级预防的实验室检查推荐的更新。新指南的推荐意见发生了明显转变:更注重成本效益,即只有当实验室检验可导致改善预后的治疗方式发生改变时,此检验才具有成本效益,才有必要去做,否则,不用作为常规检查项目。新指南将此标准应用于卒中患者的二级预防中,“对于未接受他汀治疗的急性缺血性卒中患者,无需常规进行血胆固醇的检测”。也就是说对于急性缺血性卒中患者,无论血胆固醇水平如何,均可启动他汀治疗,无需将血胆固醇水平作为判定是否启动他汀治疗的指标。
现在我们再来看看他汀作为急性缺血性卒中患者院内治疗的重要部分,新指南是怎么对其进行推荐的。
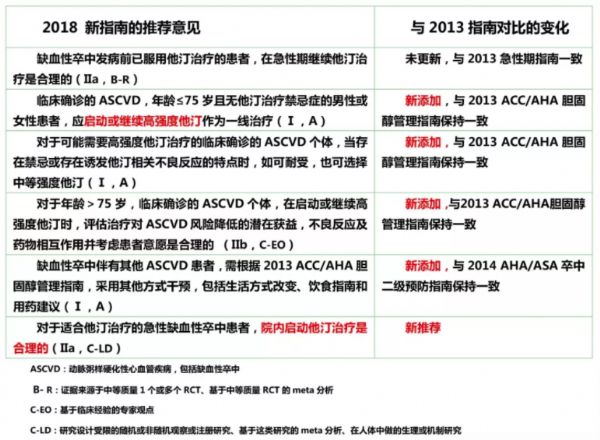
表:2018 AHA/ASA急性缺血性卒中早期管理指南关于他汀的推荐意见
由上表我们可以看出,新指南他汀治疗理念的更新主要体现在以下两点:
①强调强化理念:2013年ACC/AHA胆固醇管理指南首次将缺血性卒中划归为ASCVD范畴,推荐高强度他汀治疗。随后多部指南发布,一致强调强化他汀治疗理念。基于此,2018新指南指出:对于缺血性卒中患者,年龄≤75岁且无他汀治疗禁忌证的患者,应尽早启动或继续高强度他汀作为一线治疗。
此推荐意见的证据来源于著名的SPARCL研究。这也是迄今为止唯一针对卒中患者进行的他汀临床终点大型RCT,结果证实:高强度阿托伐他汀可使卒中复发风险显著降低16%,主要冠状动脉事件显著降低35%,任何冠状动脉事件显著降低42%。在发表后至今的12年间SPARCL研究及其亚组分析持续推动了国内外多部卒中和血脂指南的更新。
②推荐早期启动:对于急性缺血性卒中患者,若发病前已服用他汀,发病后该如何服用?新指南与2013版指南的推荐意见相同,即继续接受他汀治疗。但是,对于发病前未服用他汀的患者,何时启动他汀治疗呢?新指南首次明确指出:对于适合他汀治疗的急性缺血性卒中患者,院内及时启动他汀治疗是合理的。
那么,早期启动到底应该是卒中发病后多久启动他汀呢?一项回顾性队列研究发现,入院24小时内启动他汀治疗的缺血性卒中患者死亡风险显著低于第2天、第3天及未启动他汀治疗的患者(P<0.001)。研究表明,他汀在急性缺血性卒中患者中的治疗作用与其使用的剂量及时间有关。急性缺血性卒中,越早使用强化他汀治疗,患者获益越多!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#缺血性#
84
#缺血性卒#
68
#ASA#
69
#AHA#
93
#ISC#
78
学习了
90
^_^^_^^_^^_^
74