IBD: 溃疡性结肠炎患者在回肠袋肛门吻合全直肠切除术后维生素D缺乏常见
2022-07-11 xuyihan MedSci原创
IPAA的英文全称叫做ileal pouch anal anastomosis,这是一种能有效治疗溃疡性结肠炎的手术方式。它通过切除全部大肠以及部分肛管,再用回肠末端做成储袋。
回肠袋肛门吻合术 (IPAA) 的分期全直肠切除术 (TPC) 是合并药物难治性疾病或发育不良的溃疡性结肠炎 (UC) 患者的首选手术。新构建的储袋由回肠构成,用作替代大便储存器来代替切除的结肠和直肠。胃肠道布局的这种改变可能会影响营养物质的吸收并使患者容易营养缺乏。
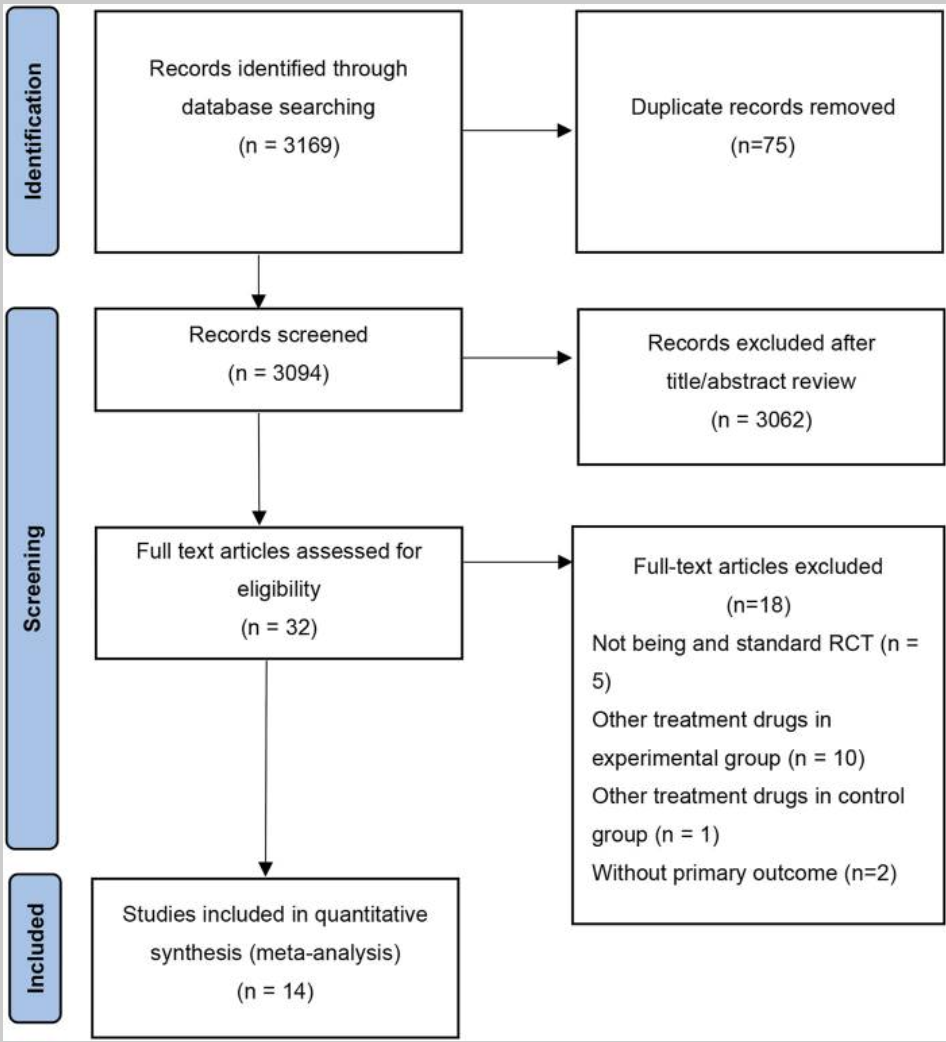
UC 患者在 TPC 与 IPAA 后的维生素 D 和骨矿物质密度较低,IPAA术后的维生素D缺乏理论上是继发于细菌过度生长、胆汁盐的过度解偶联和负责维生素D吸收的乳糜微粒的破坏。本研究的目的是扩大可用数据并证明在三级炎症性肠病 (IBD) 接受 TPC 联合 IPAA 和后续储袋镜检查的大型 UC 患者队列中维生素 D 缺乏症和低骨密度的发生率。
研究人员在一家IBD中心进行了回顾性审查,将2008年1月至2017年12月期间在西奈山医院 (MSH) 接受 TPC 和 IPAA 治疗药物难治性疾病或发育不良以及随后的储袋镜检查的所有 UC纳入本项研究。结肠切除术时年龄小于 18 岁的患者被排除在外。低维生素(Vit D)定义为<20 ng/mL 或<50 nmol/L。钙(Ca)和 磷(Phos)的低值分别定义为 <8.5 mg/dL和<2.5 mg/dL。高甲状旁腺激素(PTH)值定义为 >65 pg/mL。双能 X 线骨密度仪 (DEXA) 定义骨质减少和骨质疏松症分别定义为从 -1.0 到 -2.5 的 T 分数或 T 分数 < -2.5。

2008年1月至2017年12月期间,共有621名患者接受了TPC和IPAA,其中 412 名患者有随后的储袋镜检查数据。其中,224 人(54.3%)为男性,结肠切除术的中位年龄为 35.8 岁(IQR,26.6-49.7 岁)。在 412 名患者中,122 名 (29.6%) 测量了 Vit D,302 名 (73.3%) 测量了 Ca,144 名 (35.0%) 测量了磷,10名 (2.4%) 测量了最后一次手术后的 PTH水平。最终对14名患者 (3.4%) 进行了 DEXA 扫描,以表明先前的类固醇暴露程度。在接受和不接受上述测试的患者中,年龄、性别或结肠切除术前类固醇的使用没有显着差异。所有患者的中位Vit D水平为 27.6 ng/mL(IQR,20.1-36.8 ng/mL),在测量了Vit D的 122 名患者中,有31名(25.4%)发现了低Vit D。其中,18人(58.1%)接受了大剂量(每周 50000单位)维生素 D 补充剂。补充后12名患者 (66.7%) 重新评估了 Vit D 值,中位水平为 23.1 ng/mL (IQR, 14.4–38.6 ng/mL)。中位Ca水平为 9.3 mg/dL(IQR,9.0–9.6 mg/dL),28名患者 (9.3%) 发现低钙。20 名患者 (13.9%) 发现低磷。中位 PTH 水平为 31.0 pg/mL(IQR,19.3-50.0 pg/mL),在进行 DEXA 扫描的14名患者中,9名(64.3%)报告了骨质减少,3 名(21.4%)报告了骨质疏松症。

在这项针对接受TPC和IPAA的UC患者的大型单中心研究中,大约30%的患者测量了 Vit D,只有 3% 的患者测量了骨矿物质密度。IPAA 后维生素 D 缺乏症很常见,在进行 DEXA 扫描的一小部分患者中,骨质减少或骨质疏松症很常见。这些发现与早期研究一致,即维生素 D 缺乏和骨质减少率分别为 21.7% 和 26% 至 55%。
原始出处:
Anam Rizvi. Et al. Vitamin D Deficiency is Common in Patients with Ulcerative Colitis After Total Proctocolectomy with Ileal Pouch Anal Anastomosis. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#溃疡性#
63
#肛门#
53
#切除术#
43
#期刊论坛##学习#
66
不错的文章
61
学习一下
49
认真学习~
53
#IBD#
83
#回肠#
53