JGH: 前列腺素E主要尿代谢物可以评估溃疡性结肠炎缓解期患者的黏膜愈合情况
2022-05-16 xuyihan MedSci原创
每年大约有3万新增的确诊为克罗恩病和溃疡性结肠炎的患者;溃疡性结肠炎可以发生于任何年龄阶段;平均来说,溃疡型结肠炎好发于35岁左右。
溃疡性结肠炎 (UC) 是最常见的炎症性肠病 (IBD),近年来在欧洲和北美以及亚洲国家的发病率分别为每 10 万人505人和286人。UC 是一种特发性疾病,其特征是大肠出现溃疡由此导致生活质量下降。此外,UC 中反复出现的炎症可导致结肠癌的发生。研究显示使用内窥镜检查评估的粘膜愈合 (MH) 被称为深度缓解,并且与较少的复发和良好的预后相关。梅奥内窥镜评分 (MES) 1 的患者比 MES 0 的患者具有更高的复发风险。
临床缓解期的 UC 患者需要定期进行结肠镜检查,但由于检查时的疼痛和侵入性,不能被很好的广泛接受。前列腺素E主要尿代谢物 (PGE-MUM) 是作为前列腺素E2 (PGE2) 的代谢物会从尿中排出。在肠粘膜深部发炎的情况下,它的水平会增加。据报道,PGE-MUM 水平与 UC 中结肠炎症的程度有关。在这项研究中,研究人员评估了 PGE-MUM 在诊断 UC 的内镜、组织学和组织内镜黏膜缓解方面的有效性,并与粪便检测进行优劣性比较。

这项前瞻性研究于 2017年8月至2021年1月在韩国集庆大学医院进行。纳入计划接受结肠镜检查的处于疾病缓解期的UC患者。然后分析了患者PGE-MUM水平与内镜缓解 (ER)、组织学缓解 (HR) 和黏膜完全愈合 (CMH,定义为组织内镜缓解) 之间的关系。同时研究人员还比较了PGE-MUM、粪便钙卫蛋白 (FC) 和粪便免疫化学测试 (FIT) 之间的受试者工作特征曲线的曲线下面积 (AUC)。
本项研究总共分析了128 名患者。PGE-MUM 在内镜缓解患者与非内镜缓解患者中存在明显差异(14.5 VS 16.7,P=0.028)、而组织学缓解患者的PGE-MUM水平与非组织学缓解患者相比也更低(14.2 VS 17.4,P=0.004),和黏膜完全愈合患者相比,非黏膜完全愈合患者的PGE-MUM更高(14.3 VS 16.7,P=0.021 )。PGE-MUM、FC 的 AUC 和 ER、HR 或 CMH 的 FIT 之间没有显着差异。
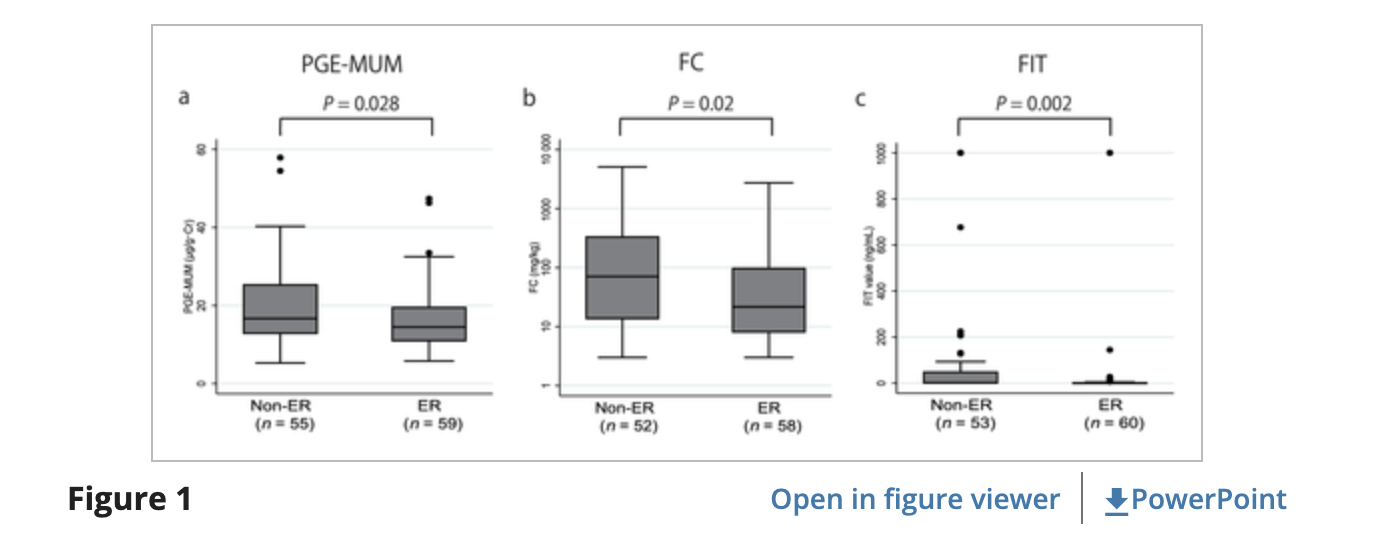
图:前列腺素E主要尿代谢物的表达水平差异
本项研究证实即使在临床缓解期间,无论疾病表型如何,PGE-MUM水平也可以确定UC患者中的黏膜完全愈合程度,表明其在无创监测方面的临床益处。
原始出处:
Toshiyuki Sakurai. Et al. Prostaglandin E-major urinary metabolite diagnoses mucosal healing in patients with ulcerative colitis in remission phase. Journal of Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#前列腺素#
58
#黏膜愈合#
48
#代谢物#
50
#缓解期#
51
#溃疡性#
36
#黏膜#
54