三星Bioepis旗下贝伐单抗生物类似物AYBINTIO获CHMP正面评价
2020-06-28 Allan MedSci原创
韩国三星Bioepis公司近日宣布,欧洲药品管理局(EMA)的人用药品委员会(CHMP)对AYBINTIO持肯定态度,该药品是贝伐单抗的生物类似物。
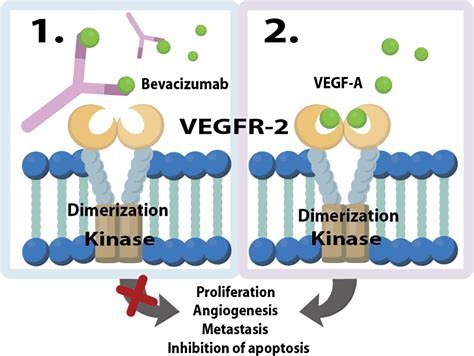
韩国三星Bioepis公司近日宣布,欧洲药品管理局(EMA)的人用药品委员会(CHMP)对AYBINTIO持肯定态度,该药品是贝伐单抗的生物类似物。CHMP推荐将AYBINTIO用于贝伐单抗的适应症,包括转移性结直肠癌(mCRC)、转移性乳腺癌(mBC)、非小细胞肺癌(NSCLC)、转移性肾细胞癌(mRCC)、上皮性卵巢癌、原发性腹膜癌和宫颈癌。欧盟委员会(EC)将对CHMP的积极意见进行审查,以决定是否授予AYBINTIO营销许可。
三星Bioepis临床科学高级副总裁Hee Kyung Kim表示:“高质量生物类似物是减轻患者经济负担的重要手段。一旦获得批准,AYBINTIO将成为针对不同类型癌症的有效治疗选择,可能会帮助欧洲的许多患者”。
AYBINTIO的市场授权申请书(MAA)得到了药代动力学(PK)和临床数据以及药理和毒理学数据的支持,这些数据表明AYBINTIO与贝伐单抗高度相似。此外,该公司于2019年9月提交了AYBINTIO的生物制剂许可申请(BLA),目前正在接受美国FDA的审查。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Bio#
77
话题
125
#CHMP#
68
#评价#
63
#贝伐#
64