Eur Heart J:既往有心肌梗塞且无冠状动脉支架置入的患者长期服用替卡格雷进行二级预防
2019-12-08 xing.T MedSci原创
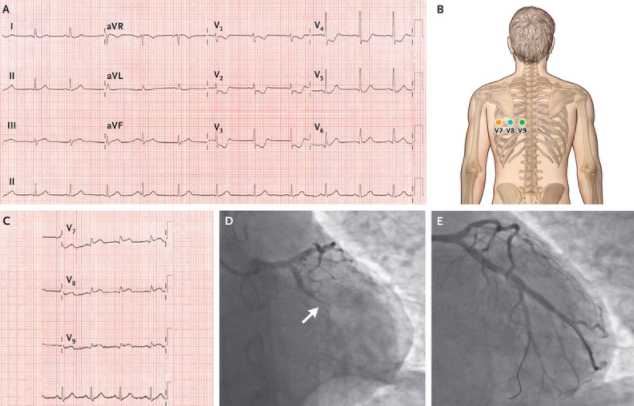
由此可见,长期服用替卡格雷可降低既往有心梗患者的血栓形成事件,无论他们是否曾进行过冠状动脉支架置入术。这些数据凸显了DAPT预防自发性动脉粥样硬化血栓形成事件的益处,并表明即使未接受支架置入治疗,高风险的既往发生MI的患者也可考虑长期服用替卡格雷治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很不错的研究发现,学习了,非常感谢
56
#冠状动脉支架#
62
学习
98
学习
103
学习
102
#ART#
40
#替卡格雷#
56
#HEART#
53
学习
95