Lancet Neurol:耐受性差,疗效阴性——不推荐贝沙罗汀治疗复发缓解型多发性硬化症(CCMR ONE)
2021-10-25 Naomii MedSci原创
研究不推荐使用贝沙罗汀治疗多发性硬化症患者,因为它的耐受性差,主要疗效结果为阴性。
多发性硬化症影响着全世界280万人,是年轻人残疾的最常见原因之一。中枢神经系统炎症导致急性脱髓鞘。虽然许多获得许可的药物有效地减轻了炎症,留下了持续性的脱髓鞘轴突,轴突失去营养支持而缓慢退化,导致进行性恶化。一个重要的未得到满足的临床需求是一种延缓或防止残疾进展的轴索再生性治疗。
保存脱髓鞘轴突最有效的策略是促进内源性再髓鞘形成。这一过程需要少突胶质前体细胞的迁移、增殖和分化,但在大多数多发性硬化症患者中最终失败。由于少突胶质前体细胞经常出现在慢性脱髓鞘多发性硬化症病变中,再髓鞘失败的部分原因可以归因于少突胶质前体细胞分化受损。为了确定能够增强这一限速阶段的治疗方法,已经进行了临床试验。
少突胶质细胞前体细胞分化的另一个积极调节因子是维甲酸X受体(RXR),它在少突胶质细胞系细胞中的重新髓鞘多发性硬化症病变中表达。抑制视黄酸受体rxr-γ(rxr-γ)信号传递可抑制啮齿动物和人类少突胶质前体细胞的分化;rxr激动剂9-顺式维甲酸可使老年大鼠脱髓鞘小脑片培养和局部毒素诱导的脱髓鞘重新髓鞘。没有获得许可的选择性rxr-γ激动剂;然而,贝沙罗汀是一种α,β和γ亚型的非选择性激动剂,已被批准用于治疗皮肤T细胞淋巴瘤。在重新髓鞘形成药物的试验中,对于最佳终点或实际治疗效果尚无共识。4种MRI序列,如磁化转移率与髓鞘含量相关,在较小程度上与轴突和胶质细胞密度相关,并允许在具有估计治疗效果的重新髓鞘形成试验中可行的样本量。当然也可以通过视觉诱发电位来评估视觉通路中重新髓鞘形成的功能后果。近日,有研究人员通过视觉诱发电位来评估视觉通路中重新髓鞘形成的效果,评估了非选择性维甲酸X受体激动剂在促进多发性硬化症患者髓鞘再生方面的安全性和有效性。
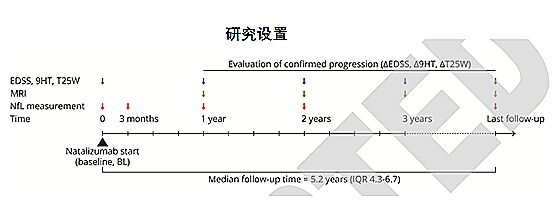
这项随机、双盲、安慰剂对照、平行分组的2a期试验(CCMR One)从英国的两个中心招募了复发-缓解型多发性硬化症患者。符合条件的参与者年龄在18-50岁之间,接受富马酸二甲酯治疗至少6个月。通过由独立统计学家运行的基于网络的系统,参与者被随机分配(1:1),通过使用四个二元因素的概率加权最小化,每天接受300毫克/平方米的口服贝沙罗汀或口服安慰剂,为期6个月。参与者、研究人员和结果评估员三盲接受治疗分配。分别在基线和6个月时进行MRI扫描。主要的安全结果是可归因于贝沙罗汀的不良事件和停药的数量。主要疗效结果是基线磁化转移率低于患者内部中位数的皮损平均磁化转移率在基线和6个月之间的患者水平的变化。分析了安全人群中的主要安全结果,其中包括接受了至少一剂分配的治疗的参与者。分析了意向治疗人群中的主要疗效结果,该人群包括所有完成研究的患者。这项研究已在ISRCTN注册中心注册,14265371,并已完成。
- 在2017年1月17日至2019年5月17日期间,52名参与者被随机分配接受贝沙罗汀(n=26)或安慰剂(n=26)。
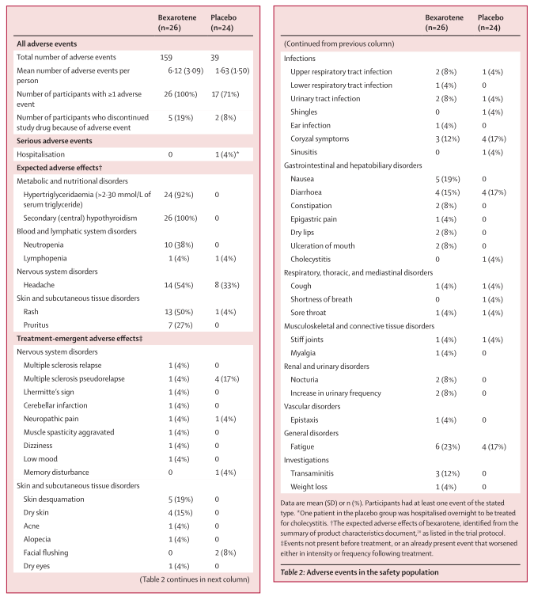
- 服用贝沙罗汀的参与者的平均不良事件数量(6·12[SD3.09];总共159个事件)高于接受安慰剂的参与者(1.63[SD1.50];总共39个事件)。
- 所有接受贝克沙罗汀治疗的参与者至少有一个不良事件,包括中枢性甲状腺功能减退(n=26比安慰剂组没有),高甘油三酯血症(n=24比没有安慰剂组),皮疹(n=13比安慰剂组)和中性粒细胞减少(n=10比没有安慰剂组)。
- 5名服用贝沙罗汀的受试者(19%)和2名服用安慰剂的受试者(8%)因不良事件而停用研究药物。在接受安慰剂治疗的参与者中,1次胆囊炎发作是唯一严重的不良事件。
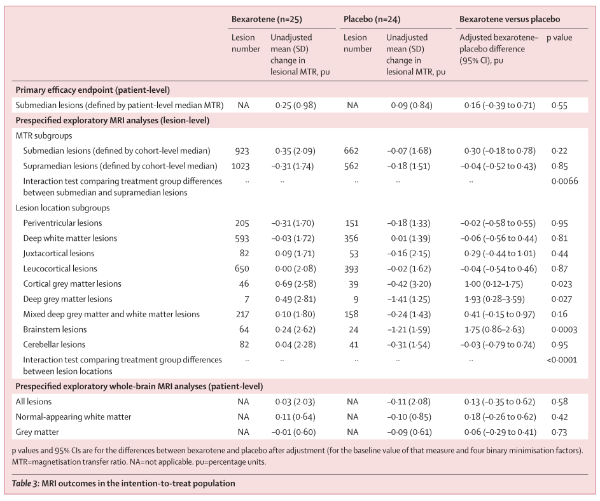
- 贝沙罗汀组(0.25个百分比单位[PU;SD 0.98])和安慰剂组(0.09PU[0.84];调整后的贝沙罗汀-安慰剂差值0.16PU,95%CI-0.39至0.71;p=0.55)的平均皮损磁化转移率变化无差异。
研究不推荐使用贝沙罗汀治疗多发性硬化症患者,因为它的耐受性差,主要疗效结果为阴性。然而,在一些探索性的MRI和电生理分析中发现了统计学上的显著性效应,这表明其他维甲酸X受体激动剂可能具有小的生物学效应,可以在进一步的研究中进行研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
74
#CMR#
75
#多发性#
61
#硬化症#
0
#贝沙罗汀#
69
#Lancet#
63
#耐受性#
120