梅斯病例报告002|剖宫产过程中的紧急行心肺分流术
2021-05-26 Oranhgy MedSci原创
感染性心内膜炎其发病率约为0.006%。本期病例报道感染性心内膜炎产妇腹产时进行开胸手术和CPB。
1.介绍
23岁,初产妇,孕27.3周,因感染性心内膜炎来院分娩。经食管超声心动图(TEE)显示主动脉瓣大片赘生物,反流加重。在引产和分娩后,患者进入心源性休克。启动了高级心脏生命支持(advanced cardiac life support,ACLS)和紧急心肺分流术(cardiopulmonary bypass, CPB)。主动脉瓣置换术已经完成。病人后来被拔掉管子并出院。
感染性心内膜炎(infective endocarditis, IE)其发病率约为0.006%。如果患者对药物治疗没有反应,可能需在怀孕期间或剖腹产(cesarean delivery, CD)时进行开胸手术和CPB。
目前,医学界尚无怀孕期间IE管理指南,其低发病率也限制了进行随机对照试验的能力。据报道,产妇死亡率高达33%,胎儿死亡率高达29%。此前有相关案例,通过成功的多学科合作,对剖腹产期间需要紧急CPB和主动脉瓣置换术(aortic valve replacement,AVR)的产妇和胎儿的结局进行了改善。
2.案例报告
23岁,初产妇,妊娠20.4周,既往无病史,因细菌性心内膜炎从外院转来。她最初到外院就诊时诉说有3天的腹痛、发热、寒战和背痛史,患者将其严重程度评为10/10。
体检时,体温为36.8℃。心脏听诊显示胸骨右缘有III/VI级收缩期射血杂音。实验室数据显示有中度正常细胞性贫血(血红蛋白8.0克/分升)和维生素B-12缺乏症。血液培养对甲氧西林敏感的金黄色葡萄球菌呈阳性。TEE显示主动脉瓣上有一个1.25×1.2厘米的球状移动性肿块,以及明显的主动脉瓣反流(见图1-3,显示主动脉瓣赘生物)。
否认使用非法药物,也没有艾滋病、乙肝或丙肝的病史。
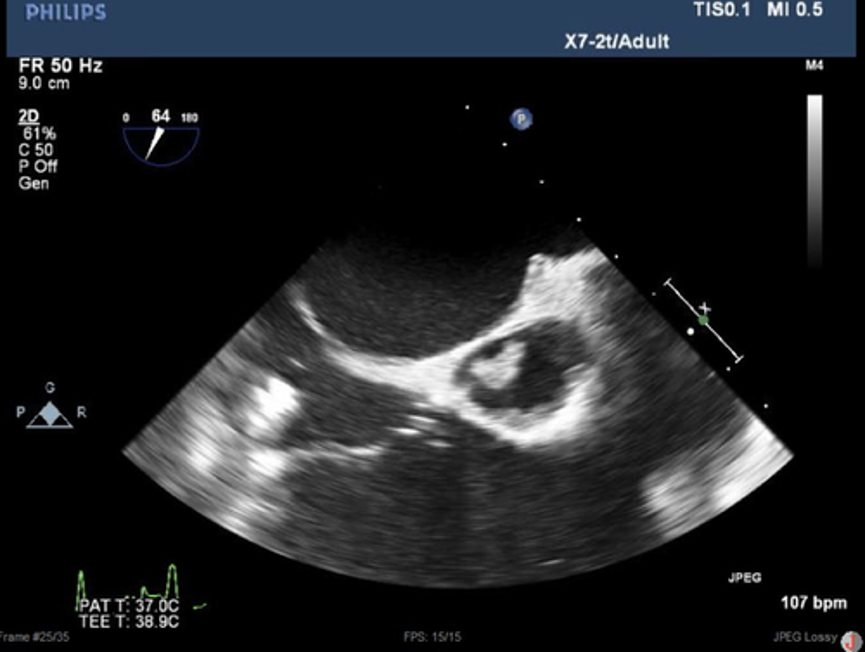
图1|右心室流入流出道的TEE图片显示非冠状动脉有大的主动脉瓣赘生物
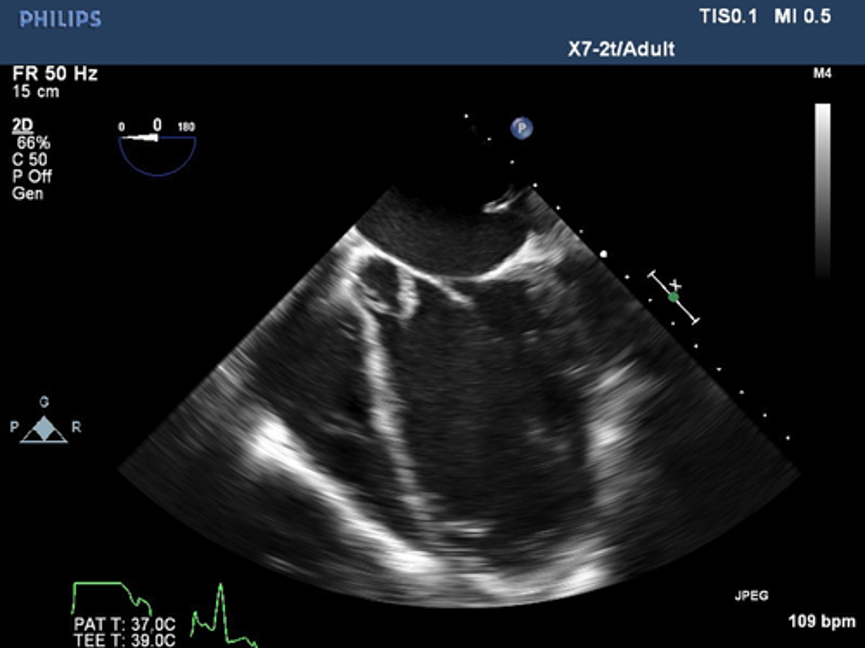
图2|五腔TEE视图的TEE图片,显示主动脉瓣的非冠状突起上附着一个赘生物

图3|TEE图片的主动脉瓣长进视图显示了轻度主动脉瓣关闭不全,这是由于附着在非冠状动脉尖上的大片赘生物所致
根据培养敏感度,开始使用纳夫西林静脉注射治疗,并计划让患者接受静脉注射抗生素至少6周。在静脉注射抗生素2周后,患者病情稳定出院,计划在门诊使用抗生素和随访。
怀孕24周时,患者因胸痛和咯血再次入院。TEE显示主动脉瓣反流已发展到严重程度(见图1-3)。鉴于指导该患者治疗的医学文献很少,因此召开了几次多学科会议,包括心胸外科医生、传染病专家、产科医生、心脏病专家、母胎医学专家、新生儿医生和麻醉师,以协调母胎护理的最佳方案。
住院期间,患者症状得到了药物控制,直到妊娠27周时,患者诉说呼吸困难加重,TEE显示在过去3周内,左心室舒张期直径从4.9厘米增加到5.6厘米,舒张期容积从157毫升增加到197毫升。
经多学科讨论后,认为决定暴发性产妇心力衰竭的风险大于胎儿早产的风险,并计划在心脏手术室进行选择性剖腹产,心胸外科医生随时待命,以防术中出现失代偿,并打算在一周后行主动脉瓣置换术。
妊娠27.3周时,患者入手术室,通过快速序列诱导,使用依托咪酯和琥珀胆碱进行环状压力诱导。在气管插管3分钟后,胎儿出生,APGARS为2/7。
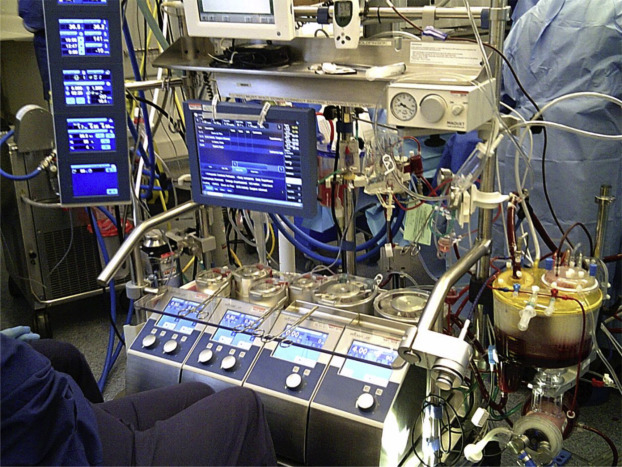
胎盘娩出后,氧饱和度立即下降到59%,平均动脉压从75mmHg明显下降到27mmHg。胸部按压开始,肾上腺素1mg静脉注射,心胸外科团队进行了紧急主动脉瓣置换。CPB是在最初的血流动力学下降18分钟后开始的,ACLS总时间为5分钟。
CPB和交叉夹闭的持续时间分别为193分钟和93分钟。在停止CPB之前,插入了主动脉内球囊泵。停止心肺分流后,病人出现严重的血管痉挛,需要输注肾上腺素、去甲肾上腺素、血管加压素和苯肾上腺素,并需要注射亚甲蓝。
患者大量输血,包括12单位PRBCs、12单位FFP、20单位冷冻血浆、2个汇集的血小板、24μg去氨加压素和7mg factor VII。
术后,转入重症监护室,安装了一个新的21mm生物假体瓣。
患者在重症监护室的术后阶段因心源性和分布性休克而变得复杂。尽管用白蛋白、血和晶体液进行了积极的容量复苏,还是出现了明显的乳酸血症,并伴有酸中毒和碱缺乏。
尽管使用了多种血管抑制剂,全身血管阻力仍保持在400-500dyn·s/cm5。最高体温为38.9°C,这与系统性炎症反应综合征(SIRS)相符。其他需要在重症监护室治疗的情况包括缺血性肝炎、急性肾脏损伤和高钠血症。
在接下来的三天里,所有的血管压缩机都被切断,在第3天,病人被成功拔管,主动脉内球囊泵(IABP)被拆除。虽然她经历了多轮ACLS,并且在心胸外科医生为CPB插管时缺乏脑部灌注,但病人没有任何神经系统的缺陷或任何其他术后病症。于术后第13天出院回家。
3 讨论
由于单靠药物治疗IE的效果有限,怀孕期间或剖腹产时的CPB可能是不可避免的。CPB对产妇和胎儿都会造成很大的发病率和死亡率,而这种高风险手术的建议和指南有限,对麻醉医生来说是很大的挑战。
在患者仍在接受抗生素治疗时,考虑早期心脏手术的原因包括由严重的主动脉或二尖瓣功能不全引起的进行性心力衰竭(HF),持续的败血症,以及防止系统性栓塞。
心力衰竭是IE最常见的并发症,随后也是最常见的手术指征。42%-60%的原生瓣膜心内膜炎病例会出现这种症状,当IE影响主动脉瓣而不是二尖瓣时,更容易出现这种症状。如果有必要在患者接受一周抗生素治疗之前进行手术,那么术后瓣膜功能障碍和复发的风险就会增加。根据诊断为IE时胎儿的胎龄,由于对母亲的健康构成威胁,考虑终止胎儿可能是合适的。
如果患有IE的孕妇必须进行手术,必须决定在怀孕期间进行手术,或在分娩时进行剖腹产与瓣膜置换和CPB联合手术。推迟分娩并进行瓣膜置换术可以使胎儿发育成熟,有可能降低早产儿的发病率和死亡率。
然而,大家都认识到CPB可因多因素的病因而导致胎儿死亡。首先,CPB可以导致胎盘低灌注,因为子宫血流不能自动调节。此外,CPB相关的低温可以刺激子宫的刺激性,并启动收缩,这可能会引起明显的血液动力学变化,并可能导致胎盘低灌注。最后,当分娩者长时间仰卧时,妊娠期子宫会压迫下腔静脉,导致胎盘功能不全和继发性胎儿缺氧。
病例报告中该产妇选择继续进行分娩和随后瓣膜置换,以最大限度地保证胎儿的安全。由于CPB需要抗凝血,剖腹产和CPB的结合严重增加了产后出血的风险。该患者出现产后出血,需要使用催产素静脉注射,甲基麦角碱IM×2,Hemabate IM×2,以及可吸收纤维素来帮助实现止血。出血量大到足以让外科医生考虑,但最终决定不采用剖腹产子宫切除术。
患者很可能因为剖腹产后胎盘自体输血而出现闪电式肺水肿并导致心力衰竭。由于为这个病例做了细致的准备,心脏外科医生在手术室里,胸部已经准备好并铺上了布,以方便紧急胸骨切开术和CPB插管。由于严重的血管痉挛综合征需要大量输血,CPB的终止被推迟了,这可能是由于长时间的心肺分流和治疗性抗凝病人的产后出血的结合。
4 结论
本病例代表了怀孕期间严重的主动脉瓣反流可能导致的临床失调。虽然以前的病例报告描述了怀孕期间IE的成功治疗,但我们的病例是独特的,因为产妇在术中急剧恶化,需要ACLS和紧急CPB。这个病例强调了多学科方法和四级产妇护理对实现最佳产妇-胎儿结果的重要性。
既往梅斯病例报告:梅斯病例报告001|非动脉炎性前部缺血性视神经病变
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心肺#
77
666
127
#梅斯#
85
#病例报告#
93
#紧急#
84
666666
107
6666666👍
97
6666
90