J Sex Med:枸橼酸西地那非与接受放射治疗前列腺癌患者的生化复发风险:一项随机对照试验的事后分析
2021-08-04 AlexYang MedSci原创
枸橼酸西地那非已证明在前列腺放射治疗(RT)的同时和之后对性功能有保护作用,但一些证据表明,前列腺根治术后服用西地那非患者的生化复发(BCR)风险增加。
枸橼酸西地那非已证明在前列腺放射治疗(RT)的同时和之后对性功能有保护作用,但一些证据表明,前列腺根治术后服用西地那非患者的生化复发(BCR)风险增加。
近期,有研究人员评估了西地那非的使用是否与接受前列腺RT患者的BCR风险增加有关,他们对一项随机安慰剂对照试验(RPCT)进行了二次分析,该试验将枸橼酸西地那非与安慰剂的治疗结局在前列腺RT期间和之后进行了比较。
研究群体由研究人员所在机构开始接受放射治疗的前列腺癌患者组成,这些患者参加了研究人员的多机构RPCT,比较了6个月的西地那非每天50毫克与安慰剂治疗,随访时间为24个月,并允许进行雄性激素阻断治疗(ADT)。前列腺癌的预后风险分组不是排除标准,但大多数研究参与者都有低或中度风险的前列腺癌。统计分析采用Kaplan-Meier图和log-rank检验。
研究人员共对162名男性的数据进行了分析。其中9名男性的PSA随访数据不足,其余153名男性纳入最终报告中。参与者的中位年龄为61岁。在8.3年的中位随访中(范围:3.0-12.2),西地那非和安慰剂组分别有5/94(5.3%)和2/59(3.4%)患者发生BCR。所有患者的6年无BCR生存率为98.8%,西地那非组为98.1%,而安慰剂组为100%。所有患者的10年无BCR生存率为94.4%,西地那非组群为95.6%,安慰剂组群为92.9%。通过对数秩比较,西地那非组和安慰剂组的无BCR生存率没有差异(P=0.36)。
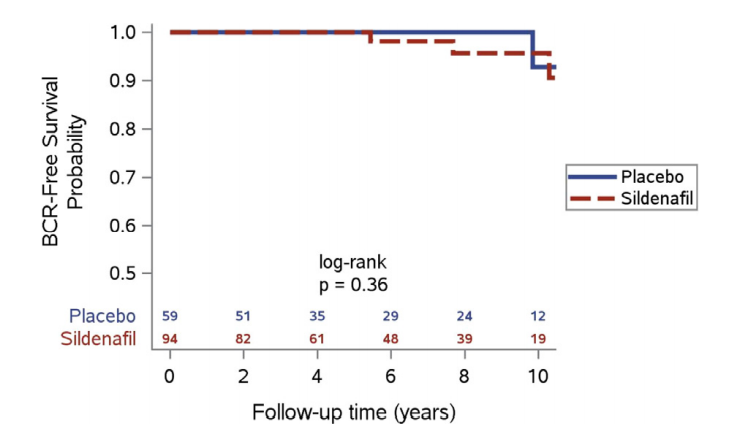
安慰剂组和西地那非组的无BCR生存
综上所述,预防性枸橼酸西地那非与放射治疗的前列腺癌患者的生化复发风险没有关系。然而,该研究无法明确得出阴性结论。该分析为临床决策提供了关于在前列腺RT期间和之后使用西地那非的安全性。研究的优势在于前瞻性、随机安慰剂对照试验中接受治疗的患者,他们的用药依从性很高。然而,研究的局限性在于分析的事后性,一些患者使用ADT,无法检测出西地那非与安慰剂组之间的BCR差异。
原始出处:
Justin M Haseltine , Margaret Hopkins , Elizabeth Schofield et al. Sildenafil Citrate and Risk of Biochemical Recurrence in Prostate Cancer Patients Treated With Radiation Therapy: Post-Hoc Analysis of a Randomized Controlled Trial. J Sex Med. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#对照试验#
92
#复发风险#
81
#对照#
114
#随机对照试验#
88
#生化复发#
87
#Med#
77
高质量研究,读起来真爽,谢谢梅斯
0
前列腺癌相关研究,学习了,谢谢梅斯
99