Cell:发现清除衰老细胞的新机制!这种人体中的病毒是关键!
2023-05-12 吴武陵 生物探索 发表于上海
人体组织内广泛存在一种病毒,而免疫系统对该病毒的反应,可以帮助检测和清除皮肤中的衰老细胞。
随着年龄的增长而出现的衰老细胞虽丧失了分裂能力,却并不一定会及时死亡。这些衰老细胞在人体内逐渐积累,将引发慢性炎症,甚至导致癌症和退行性疾病等病症。已有研究表明,在小鼠身上,清除老化组织中的衰老细胞可以恢复组织平衡,并延长健康寿命。
近日,麻省总医院(Massachusetts General Hospital,MGH)的一个研究小组发现,人体组织内广泛存在一种病毒,而免疫系统对该病毒的反应,可以帮助检测和清除皮肤中的衰老细胞。3月30日,该研究结果以“Cytotoxic CD4+ T cells eliminate senescent cells by targeting cytomegalovirus antigen”为题发表在Cell上。

图1 研究成果(图源:[1])
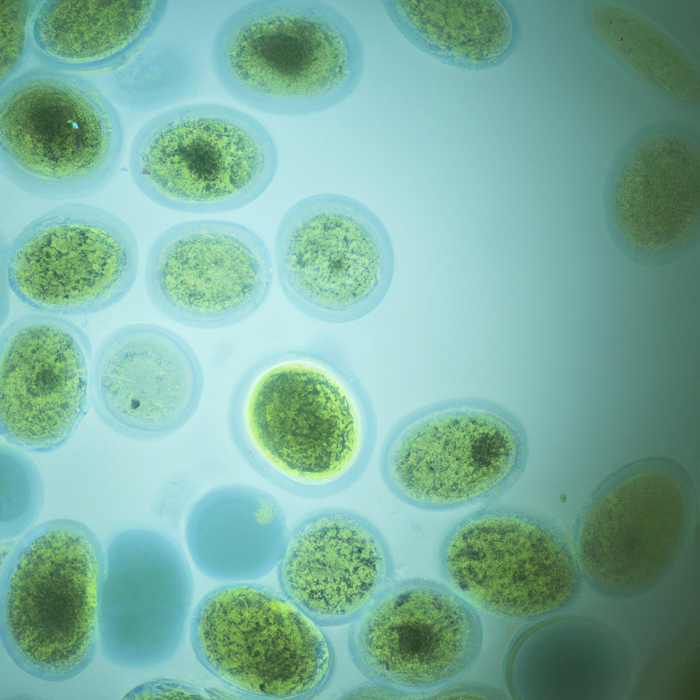
科学家们分析了年轻和老化的人体皮肤样本,以了解人体组织中衰老细胞的清除情况。研究人员发现,老化的皮肤样本中衰老细胞比年轻样本中的衰老细胞更多,尤其表现为真皮细胞中衰老标志物p16INK4a阳性细胞的增加。然而,在老年人的样本中,衰老细胞的数量并未与个体年龄的增长呈显著相关性,这表明存在某种机制能够控制它们的数量。
在排除了表皮状况、血液或淋巴管密度等因素后,实验发现,某些免疫细胞,即杀手CD4+ T细胞,其数量与真皮衰老细胞数量呈最负相关。这表明,CD4+ T细胞在阻止衰老细胞增加中起到关键作用。研究人员还发现,角质形成细胞表达的CXCL9趋化因子可能导致CD4+ T细胞募集到皮肤,并完成衰老细胞的清除。
在评估杀手CD4+ T细胞如何控制衰老细胞时,研究人员发现,衰老的皮肤细胞会表达一种人类巨细胞病毒产生的蛋白质或抗原。人类巨细胞病毒是一种普遍存在的疱疹病毒,在大多数人体内建立终生潜伏感染而不出现任何症状。一旦表达这种蛋白质,衰老细胞就成为了杀手CD4+ T细胞攻击的目标,接下来发生的事,就和免疫应答没什什么两样了。
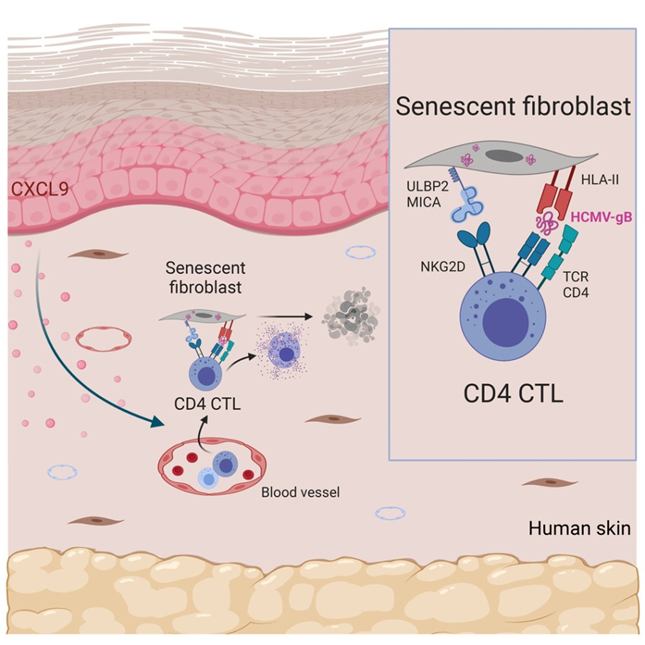
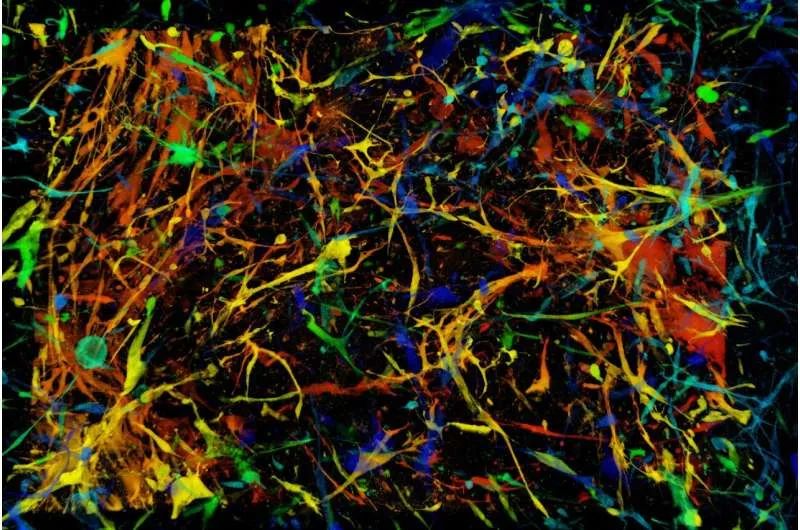
图2 利用免疫系统对人类巨细胞病毒反应,清除衰老细胞(图源:[1])
研究的资深作者、MGH 高危皮肤癌诊所主任、皮肤病学副教授Shawn Demehri博士表示:“我们的研究表明,人类巨细胞病毒的免疫反应有助于维持衰老器官的平衡。我们大多数人都感染了人类巨细胞病毒,我们的免疫系统则进化出了清除表达巨细胞病毒抗原细胞的能力,其中也包括对衰老细胞的清除。”
这些发现突显了人体内存在病毒的有益功能及其临床应用的潜力。Demehri表示:“我们的研究为通过增强抗病毒免疫反应消除衰老细胞的新治疗方法提供了可能。我们对利用巨细胞病毒的免疫反应作为治疗癌症、纤维化和退行性疾病中消除衰老细胞的疗法抱有极大的兴趣。这项研究也可能在美容皮肤学方面取得进展,例如开发使皮肤看起来年轻的新疗法。”
参考资料:
[1]Tatsuya Hasegawa, Tomonori Oka, Heehwa G. Son, et al, Cytotoxic CD4+ T cells eliminate senescent cells by targeting cytomegalovirus antigen, Cell (2023). DOI: 10.1016/j.cell.2023.02.033
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习,共同进步
74
学习
0
不错,学习了。
102
学习了,谢谢分享
66
谢谢分享
97