European Radiology:这一影像学指标,成为了急性卒中出现恶性脑水肿的新兴预测手段!
2022-04-07 shaosai MedSci原创
Alberta卒中项目早期CT评分(ASPECTS)是一个半定量的评分系统,可评估CT图像上的梗死程度、缺血性改变的程度以及大脑中动脉(MCA)区域内的局灶性肿胀。

脑水肿(CED)是缺血性卒中大血管闭塞(LVO)的一个重要并发症,不及时干预常会导致多种并发症的出现。恶性脑水肿(MCE)在发病后2至5天达到高峰,可导致不可逆的组织损伤、脑血流不足、颅内压升高,甚至脑疝。因此,确定CED的早期风险因素可有助于提高MCE患者的预后。
目前,监测水肿发展的评估需要密切关注临床神经系统症状的恶化,高危患者可能出现新的或严重的意识障碍以及新的瞳孔异常或对疼痛的反应减弱,但这些症状都较为主观。
最近,来自非增强CT(NECT)的定量病变净水摄取量(NWU)成为评估缺血性水肿和功能预后的新兴预测指标。然而,NWU的应用要求梗死区域清晰可见,但大多数CT图像对梗死区域的显示都是模糊的,因此限制了其在临床上的广泛应用。
Alberta卒中项目早期CT评分(ASPECTS)是一个半定量的评分系统,可评估CT图像上的梗死程度、缺血性改变的程度以及大脑中动脉(MCA)区域内的局灶性肿胀。现阶段,临床上引入了人工智能和机器学习的自动-ASPECTS软件对CED进行评估。多项研究表明,自动-ASPECTS比视觉评价增加了检测早期缺血性变化的可靠性。
近日,发表在European Radiology杂志的一项研究利用自动-ASPECTS技术,在基线多模态CT(NECT和CTA-SI)上自动检测到的急性脑缺血区的患者中对NWU进行测量,探讨了基线ASPECTS-NWU预测随后出现MCE的诊断价值,并与临床变量进行了比较。
本研究共纳入了146名出现大血管闭塞的患者。基于自动ASPECTS的定量NWU在非增强CT(NECT)和CT血管成像(CTA)上都进行了测量,即NECT-ASPECT-NWU和CTA-ASPECTS-NWU。ASPECTS-NWU与脑水肿(CED)等级之间的相关性采用Spearman等级相关法计算。采用单变量逻辑回归法评估放射学和临床特征对MCE的影响,并建立了包含单变量回归分析中显著因素的多变量模型。得到受试者工作特征(ROC)并比较了曲线下面积(AUC)。
CTA-ASPECTS-NWU与CED等级呈中度正相关(r = 0.62;95%置信区间[CI],0.51-0.71;p < 0.001)。CTA-ASPECTS-NWU比NECT-ASPECTS-NWU表现更好,AUC 0.88 vs. 0.71(p < 0.001)。整合了CTA-ASPECTS-NWU、附属评分和年龄的多变量逻辑回归模型显示,CTA-ASPECTS-NWU是MCE的独立预测因素,AUC为0.94(95%CI:0.90-0.98;P<0.001)。
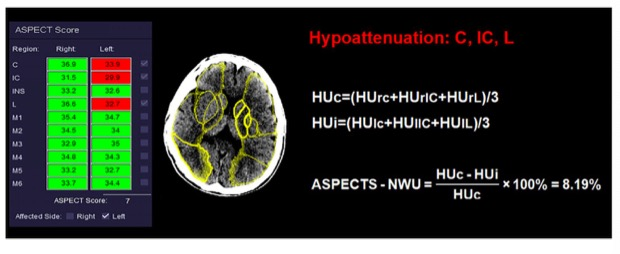
图 62岁男性,在发病4小时后进行影像学成像。自动ASPECTS软件确定低密度区域为C、IC和L。根据公式,ASPECTS-NWU为8.19%
本研究表明,对入院时NECT和CTA-SI进行的自动-ASPECTS量化所产生的早期受影响区域的NWU可以对具有急性LVO后发生脑水肿风险的患者进行早期识别。此外,CTA-ASPECTS-NWU是MCE的一个独立预测因素,这为该类患者的早期治疗及预后评估提供了便捷的技术支持。
原文出处:
JiaQian Shi,Hang Wu,Zheng Dong,et al.Automated quantitative lesion water uptake in acute stroke is a predictor of malignant cerebral edema.DOI:10.1007/s00330-021-08443-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
74
#脑水肿#
70
#急性卒中#
80
#水肿#
88