Nat Med:mitoTALENs技术能消除线粒体内DNA突变
2013-08-10 MedSci MedSci原创
美国的研究人员开发出一种新方法来清除线粒体内的突变DNA,从而有望治疗多种线粒体病。据介绍,这也是TALENs技术首次用于线粒体基因的编辑。这项研究成果于8月4日在线发表在Nature Medicine上。 日前,迈阿密大学米勒医学院(University of Miami Miller School of Medicin
美国的研究人员开发出一种新方法来清除线粒体内的突变DNA,从而有望治疗多种线粒体病。据介绍,这也是TALENs技术首次用于线粒体基因的编辑。这项研究成果于8月4日在线发表在Nature Medicine上(PDF文件下载)。
日前,迈阿密大学米勒医学院(University of Miami Miller School of
Medicine)的研究人员利用TAlENs技术首次清除线粒体内的突变DNA,以使得突变的线粒体DNA下降了,这项研究有望用于治疗母系遗传的线粒
体病。研究成果发表在Nature Medicine上。
线粒体病通常是由突变的线粒体DNA(mtDNA)引起的,在大部分情况下它与野生型mtDNA共同存在,导致mtDNA异质性。常见的线粒体病包括线粒
体肌病、线粒体脑病和线粒体脑肌病,如Leber遗传性视神经病(LHON)。这种疾病的主要症状为视神经退行性病变,在男性中较多见。
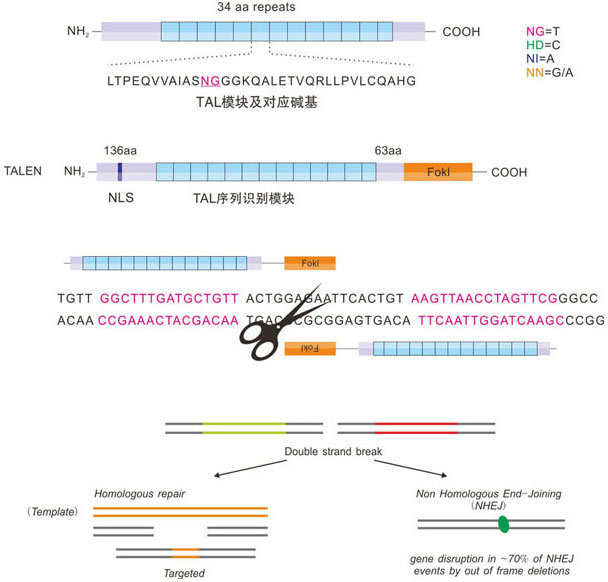
TALENs技术路线图
TALENs清除突变的线粒体基因
在这项研究中,迈阿密大学米勒医学院的研究人员探索了转录激活因子样(TAL)效应物,同时在寻找修复线粒体基因缺陷的新策略。他们尝试了TAL效应物核酸酶(TALENs)这种基因编辑的新方法。
研究人员在实验室中使用细胞来设计线粒体靶向的TALENs(mitoTALENs),来结合并切割线粒体DNA,正是这段基因中的一个突变引起了 LHON.他们随后检测了mitoTALENs是否清除了mtDNA.分析结果表明,细胞中总的mtDNA暂时下降,这是由于突变mtDNA的下降。
文章的通讯作者,神经和细胞生物学教授Carlos T. Moraes博士表示:"一旦mitoTALENs与特定靶点的DNA结合并切割,突变的mtDNA就被降解。总的mtDNA的下降刺激细胞通过复制未受 影响的分子来增加其mtDNA.两周之后,mtDNA水平恢复正常。但由于突变的mtDNA被破坏,细胞中大部分为正常的mtDNA."
Moraes博士提到,清除细胞中的大部分但并非全部突变mtDNA已足以治疗多种线粒体病,因为只有当突变mtDNA占了80%以上时,它才会引起疾病的症状。研究人员计划下一步在动物中检验这种方法。
TALENs是近年来发展迅速的编辑基因
TALENs作为一种全新的基因组编辑工具,近年来引起了人们的极大兴趣。与ZFN相比,它更便宜,更高效,脱靶率低。利用这种技术,研究人员已经开发出多种疾病的动物模型,有助于疾病的分子机制研究。
在研发TALENs技术过程中,科研人员发现来自植物病原菌Xanthomonas中的TAL蛋白核酸结合域的氨基酸序列与其靶位点的核酸序列有较恒定的 对应关系。利用此恒定对应关系,构建与核酸内切酶的融合蛋白,在特异位点打断目标基因组DNA序列,从而可在该位点进行DNA编辑修饰操作,比如 knock-out、knock-in、碱基替换、点突变或者基因修饰等。该技术能识别任意目标基因序列,不受上下游序列影响等问题,因此使得基因操作更 加简单方便。
原始出处:
Bacman SR, Williams SL, Pinto M, Peralta S, Moraes CT.Specific elimination of mutant mitochondrial genomes in patient-derived cells by mitoTALENs.Nat Med. 2013 Aug 4. doi: 10.1038/nm.3261
下载:PDF文件
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#MIT#
82
#Total#
136
#Nat#
71
#DNA突变#
87
#Med#
105