Neurology:急性卒中取栓术后蛛网膜下腔高密度的双能CT特征——弥漫性模式与较差临床预后相关
2022-01-04 Naomi MedSci原创
近日,有研究人员通过使用介入后双能CT评估MT后SA-HD的发生率、特点、临床相关性和预测因素。在接受机械取栓治疗的颈动脉近端闭塞患者中,介入后8小时影像学上弥漫性SA-HD与90天较差临床预后相关。
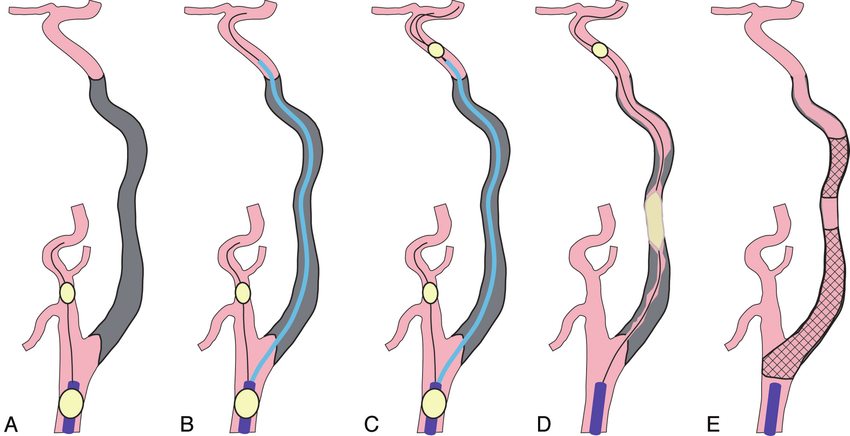
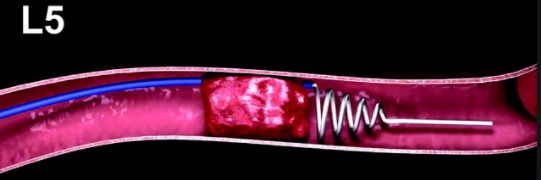
动脉破裂引起的介入后蛛网膜下腔高密度(SA-HD)是机械血栓切除术(MT)后比较常见的发现。SA-HD在多达24%的治疗患者的早期随访CT扫描中被发现,通常位于治疗血管的同侧半球。在常规CT扫描中,很难区分碘化造影剂引起的高密度与血液外渗相关的高密度。双能CT(Dual Energy CT,DE-CT)是一种基于正常脑组织、碘和血液在不同照射能量水平下的不同衰减效应的技术,它可以可靠地区分不同脑室(包括脑实质和颅内外间隙)因碘对比渗出或出血而产生的高密度。从机理的角度来看,考虑到碘和血细胞成分的分子量不同,根据其含量分割轴外高密度可以早期对血脑屏障和血液进行定性分级。
移植后SA-HD的临床影响尚不确定。虽然孤立性蛛网膜下腔出血(SAH)似乎是无害的,弥漫性蛛网膜下腔出血或SAH合并实质血肿与较差的临床预后相关。然而,精细区分血液和造影剂渗出可能改善MT治疗急性卒中患者MT后SA-HD的预后意义的评估。近日,有研究人员通过使用介入后双能CT(DE-CT)评估MT后SA-HD的发生率、特点、临床相关性和预测因素。
研究人员回顾了单中心连续一系列接受MT治疗的急性卒中患者。治疗后的SA-HD定义为在MT后8小时内进行的随访DE-CT中出现的轴外高密度。SA-HD根据其内容(孤立对比渗出与血液外渗)和范围[弥漫性(多个间隔区内高密度)与非弥漫性(高密度)]进一步分类。调整后的Logistic回归模型评估了SA-HD与治疗前和程序变量以及不良的临床结果(90天后在有序的Rankin量表中向更差的类别转变)之间的关系。
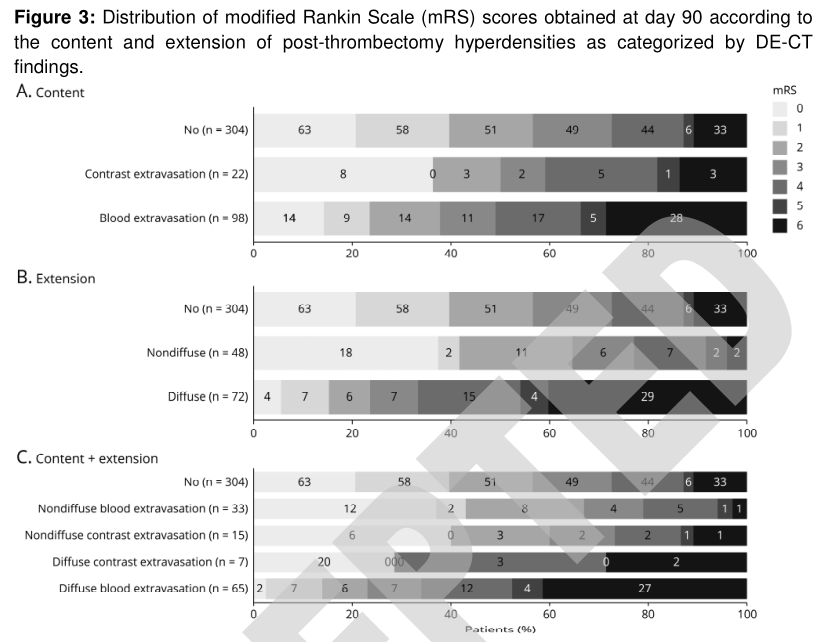
- 424例患者中120例(28%)出现SA-HD,其中单纯造影剂渗出22例,血液渗出98例。本组SA-HD弥漫性72例(60%),其中单纯造影剂外渗7例,血外渗65例;非弥漫性48例(40%),单纯造影剂外渗15例,血外渗33例。
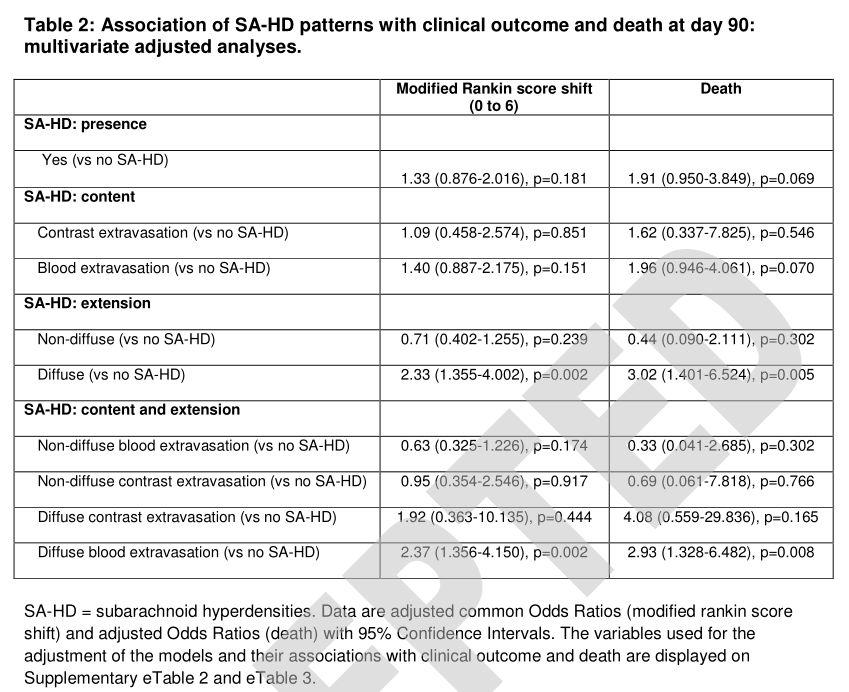
- 弥漫性SA-HD在调整后的模型中与较差的临床结局显著相关(COR=2.3,95%CI=1.3-4.00,p=0.002),而不是单独使用特定的SA-HD含量。
- 与无SA-HD相比,只有弥漫性渗血模式与较差的临床结局显著相关(COR=2.495%CI=1.36~4.15P=0.002)。
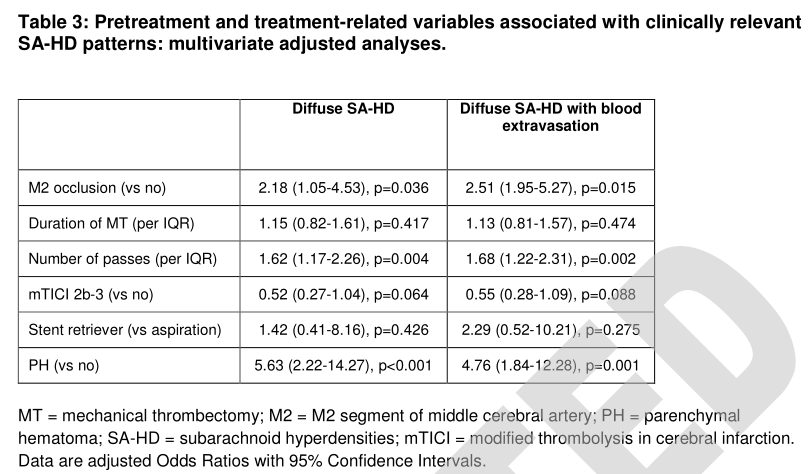
- 弥漫性SA-HD模式可通过M2闭塞、更多的血栓清除次数和并发实质血肿来预测。
在该队列患者中,MT后中位数8小时内成像,介入后SA-HD在17%的血栓摘除术中显示为弥漫性模式,并与更繁琐的操作相关。弥漫性SA-HD而不是局部采血或造影剂渗出与不良结局和死亡的风险增加相关。这些发现加强了再灌注策略改进的必要性。
这项研究提供了II类证据,在接受机械取栓治疗的颈动脉近端闭塞患者中,介入后8小时影像学上弥漫性蛛网膜下腔高密度与90天后的临床结果较差相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#蛛网膜#
84
#Neurol#
72
#双能CT#
85
#取栓术#
86
涨知识了
91
好
92
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
89
学习
126
学习
91
学习了
77