NEJM:腹腔镜与开放性剖腹手术治疗直肠癌无差异
2015-04-04 MedSci译 MedSci原创
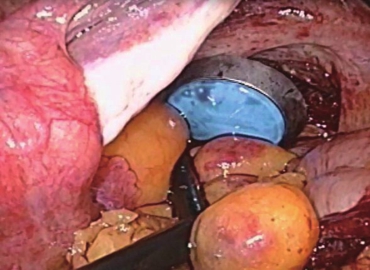
背景:使用腹腔镜切除术治疗直肠癌已被广泛应用。然而,强劲证据表明,腹腔镜手术与开放性剖腹手术在治疗直肠癌有相似的预后和局限性。我们设计实验比较三年来接受腹腔镜手术或开放性剖腹手术后直肠癌患者复发并转移至盆腔或会阴部位(局部转移)的情况和生存情况。方式:在这项涉及30家医院的国际性实验中,我们随机分配距肛周15cm以内的单一直肠腺癌患者(肿瘤不侵犯邻近组织,不发生远处转移)接受腹腔镜手术或开放性剖腹
背景:
使用腹腔镜切除术治疗直肠癌已被广泛应用。然而,强劲证据表明,腹腔镜手术与开放性剖腹手术在治疗直肠癌有相似的预后和局限性。我们设计实验比较三年来接受腹腔镜手术或开放性剖腹手术后直肠癌患者复发并转移至盆腔或会阴部位(局部转移)的情况和生存情况。
方式:
在这项涉及30家医院的国际性实验中,我们随机分配距肛周15cm以内的单一直肠腺癌患者(肿瘤不侵犯邻近组织,不发生远处转移)接受腹腔镜手术或开放性剖腹手术,且二者人数比例大约为2:1.我们关注的主要指标是术后3年内肿瘤局部复发的患者人数,我们关注的次要指标是康复患者和所有生存的患者人数。
结果:
一共1044名患者参与了实验,其中有699名患者接受腹腔镜手术,我们称之为实验组,有345名患者接受了开放性剖腹手术,我们称之为对照组。实验表明,3年内,两组患者术后局部肿瘤复发率为5.0%(差异为0,90%可信区间为-2.6到2.6);在实验组中,康复痊愈患者所占比例为74.8%,在对照组中,康复痊愈患者比例占70.8%(差异为4.0%,95%可信区间为-1.9到9.9).且在实验组和对照组中患者存活率分别为86.7%和83.6%(差异为3.1%,95%可信区间为-1.6到7.8).
结论:
实验结果表明,若对直肠癌患者进行手术,使用腹腔镜术或者开放性剖腹手术后,二者在患者术后肿瘤复发、治愈、生存情况等方面无明显差异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











不错,学习了
95
#腹腔镜#
34
#手术治疗#
37
学习,很受用
120
已阅
111
是吗?
131
是不是意味着两者的效果无差异?
75