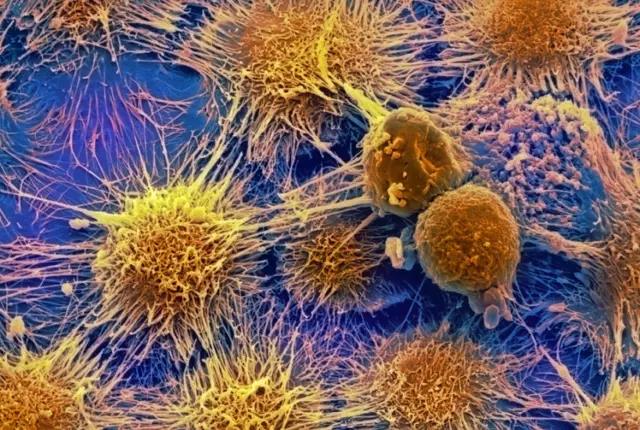
Sci Rep:血浆外泌体miR-125a-3p可作为早期结肠癌的诊断生物标志物
2017-08-06 MedSci MedSci原创
循环系统中外泌体在用于作为疾病的诊断和预后的生物标志物具有极大的潜力。本实验组既往研究中使用miRNA测序识别了异常表达的外泌体miRNA,将其作为结肠癌患者的候选诊断标志物。为验证此发现,本研究纳入了50名早期结肠癌患者和50名匹配的健康志愿者。分离其血浆来源的外泌体miRNA。实时定量PCR显示,早期结肠癌患者血浆外泌体的miR-125a-3p和miR-320c明显升高。ROC曲线显示,曲线下
循环系统中外泌体在用于作为疾病的诊断和预后的生物标志物具有极大的潜力。本实验组既往研究中使用miRNA测序识别了异常表达的外泌体miRNA,将其作为结肠癌患者的候选诊断标志物。
为验证此发现,本研究纳入了50名早期结肠癌患者和50名匹配的健康志愿者。分离其血浆来源的外泌体miRNA。实时定量PCR显示,早期结肠癌患者血浆外泌体的miR-125a-3p和miR-320c明显升高。ROC曲线显示,曲线下面积(AUC)为68.5%, CEA为83.6% ,表明miR-125a-3p的水平可预测结肠癌的发生。结合miR-125a-3p和CEA可将AUC提高至85.5%。此外,血浆外泌体miR-320c 和miR-125a-3p的水平与神经浸润显著相关(P< 0.01),而与肿瘤大小、浸润深度及分化程度无关(P > 0.05)。相反,血清CEA的水平则与肿瘤大小、浸润深度及分化程度相关,(P<0.05,r= 0.3009 –0.7270),但与神经浸润无关(P = 0.744 )。
总之,该研究结果表明,血浆外泌体miR-125a-3p或可作为早期结肠癌的诊断生物标志物。与传统的诊断标志物结合时可提高诊断率。
原始出处:
Jing Wang, Feihu Yan, et al., Circulating exosomal miR-125a-3p as a novel biomarker for early-stage colon cancer. Sci Rep. 2017; 7: 4150. Published online 2017 Jun 23. doi: 10.1038/s41598-017-04386-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#miR#
49
#标志物#
57
#血浆外泌体#
69
#生物标志#
47
#生物标志#
51
学习了,谢谢分享
79
好好文章学习了
70
学习了,好文章
92
henhao
70
好
70