本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

2016-06-17 潇潇 医学界肿瘤频道
ASCO大会三阴性乳腺癌及乳腺外科领域的热点体会。

2016年美国临床肿瘤协会年会(ASCO)召开,制药巨头礼来在会议上公布了CDK4/CDK6抑制剂abemaciclib在HR+/HER2-转移性乳腺癌中的II期临床试验结果。该项名为MONARCH 1的临床试验数据由纪念斯隆凯特琳癌症中心的Maura Dickler口头汇报展示。 MONARCH1是一项单臂临床研究,纳入了132名此前接受过一到两种化疗以及激素治疗方案并发生疾病进展的HR+/H
英国一位女士Alison Dagul被诊断为侵略性的乳腺癌和卵巢癌,经过血液测试后发现病因是基因缺陷。她不仅从父亲那里继承了这种基因缺陷,而且检测结果表明这种基因缺陷还遗传给了自己的女儿——24岁的Gaby。父亲携带基因突变 致女儿患癌Alison表示:“在得知癌症诊断结果的几个星期前,我还是一个健康的50岁妇女。我曾看着自己的儿女长大成人,并期待着与我的丈夫安东尼共度美好的晚年。但是突然间,
Abstract 5501 Study19研究:Olaparib治疗BRCA突变铂敏感复发的浆液性卵巢癌的总生存期(OS)数据更新报道 Oral Abstract Session 背景: II期研究Study19显示,olaparib维持治疗对比安慰剂,可以显著延长铂敏感复发的高级别浆液性卵巢癌患者的无进展生存期(PFS),其中BRCA1/2基因突变(BRCAm)的患者接受ola
在瑞士有超过5700名妇女被诊断为乳腺癌,每年几乎有1400名患者死于该病。许多入侵形式的乳腺癌中的癌细胞表面有很多HER2受体,这将导致癌细胞不受控制的生长发展。有很多种抗体如曲妥珠单抗和帕妥珠单抗可以识别HER2受体,这在乳腺癌治疗中已经使用许多年了。然而,这些抗体不能杀死癌细胞。相反,癌细胞可以使它们处于休眠状态,这样癌细胞在任何时间里都可以自由生长复制。 为什么抗体治疗对乳腺癌细胞无
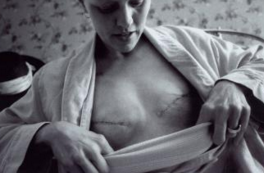
大约8名女性中就有一人将在她的一生当中患上浸润性乳腺癌。这可能是使用人工合成性激素和其他环境因子导致的,也可能是BRCA1基因等发生突变导致的。平均而言,BRCA1基因发生突变的女性有高达87%的风险患上乳腺癌。截至目前,预防性手术切除是显著降低乳腺癌风险的唯一方法,但是这也经常伴随着术后并发症。2010年,奥地利科学院分子生物技术研究所(IMBA)科学主任Josef Penninger和他的
在激素受体阳性的早期乳腺癌的绝经后女性患者中,用芳香酶抑制剂前期单一治疗5年或在他莫昔芬治疗后治疗是首选的治疗方法。用芳香酶抑制剂延长10年治疗可进一步减少乳腺癌复发的风险。原始出处:Paul E. Goss,James N. Ingle,Kathleen I. Pritchard,et al.Extending Aromatase-Inhibitor Adjuvant Therapy to 10


梅斯医学MedSci APP
医路相伴,成就大医
#ASCO2016#
114
#ASC#
62
好文章,值得学习
176
女人的天敌
150
赞
128
不知道没什么
215