Sic transl med:血小板通过调节髓系抑制因子加速动脉粥样硬化进展
2019-11-08 QQY MedSci原创
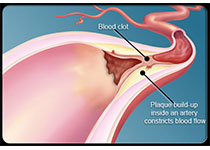
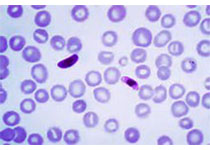
众所周知,血小板是止血和血栓形成的介质,但其炎症效应特性越来越多的被揭示出来。动脉粥样硬化,一种慢性血管炎性疾病,代表了动脉壁脂质沉积与未解决的炎症之间的相互作用。近期,研究人员发现血小板可诱导单核细胞迁移和招募到动脉粥样硬化斑块,导致斑块血小板-巨噬细胞聚集。在以西方膳食(高脂饮食)喂养的Ldlr-/-小鼠中,耗竭血小板可减小斑块的大小和坏死区,并可减少巨噬细胞积累。血小板通过使斑块巨噬细胞向炎
近期,研究人员发现血小板可诱导单核细胞迁移和招募到动脉粥样硬化斑块,导致斑块血小板-巨噬细胞聚集。在以西方膳食(高脂饮食)喂养的Ldlr-/-小鼠中,耗竭血小板可减小斑块的大小和坏死区,并可减少巨噬细胞积累。
血小板通过使斑块巨噬细胞向炎症表型倾斜、增加细胞因子信号3 (SOCS3)的髓系抑制因子的表达和降低Socs1: SOCS3的比值来驱动动脉粥样硬化形成。血小板诱导的Socs3表达通过促进炎性细胞因子(Il6、Il1b和Tnfa)的产生和削弱吞噬细胞能力来调节斑块巨噬细胞的重编程,使其功能障碍进而导致未解决的炎症和持续的斑块生长。
在心血管疾病人类患者中,研究人员发现与无心肌梗死的女性相比,有心肌梗死的女性的SOCS3的表达上调、SOCS1:SOCS3比值减小、单核细胞-血小板聚集增多。一个关于下肢动脉硬化患者的次级队列表明,SOCS3和SOCS1:SOCS3比值与血小板活性和炎症相关。
总而言之,本研究揭示了血小板介导的髓系炎症和功能障碍、SOCS3和心血管疾病之间的因果关系,明确了血小板的促动脉粥样硬化作用,并强调了在没有血栓形成的情况下,血小板如何促进炎症。
原始出处:
Tessa J. Barrett, et al.Platelet regulation of myeloid suppressor of cytokine signaling 3 accelerates atherosclerosis.Science Translational Medicine. 06 Nov 2019:Vol. 11, Issue 517, eaax0481. DOI: 10.1126/scitranslmed.aax0481
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#髓系抑制因子#
29
#粥样硬化#
38
#Transl#
28
#TRA#
33
#抑制因子#
47
#Med#
22