阿司匹林一级预防,NEJM和Lancet上多项试验纷纷Say No
2018-10-21 医咖会 医咖会
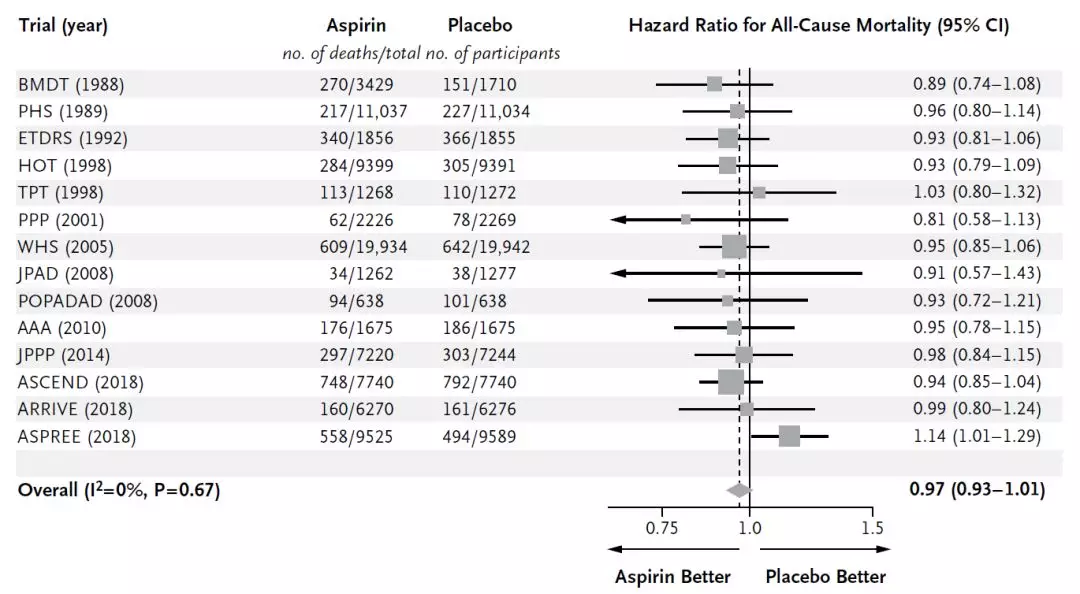
阿司匹林用于心血管事件二级预防的有效性已经得到了明确的证实。随后又出现了一系列大规模的一级预防试验,包括Physicians’ Health Study和 Women’s Health Study,显示对高风险患者有低到中等程度的益处。然而阿司匹林的这些早期预防试验所在的时期,吸烟很常见,多数血压控制不佳,强化降脂也很少见。因此,预防性使用阿司匹林的风险和益处仍然不明确,应该使用的剂量和持续时
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
53
学习了,很有用
87
学习了
101
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
93
好好好好好好好好
93
学习了
86
学习了
0