Sci Transl Med:会“呼吸”的组织密封剂!可粘合动脉血管壁!
2017-10-06 Juka 转化医学网
在外科手术中,外科医生为了修复破裂或刺穿的器官和组织,往往会选择使用缝合钉,缝合线或者电刀将伤口边缘缝合或者黏合在一起,以使它们能够愈合。
在外科手术中,外科医生为了修复破裂或刺穿的器官和组织,往往会选择使用缝合钉,缝合线或者电刀将伤口边缘缝合或者黏合在一起,以使它们能够愈合。
然而,这些措施在身体的某些难以到达的部位就很难去操作,并且这些伤口通常无法使用这些手段立即完全密封,从而可能导致组织存在进一步损坏和感染的风险。比如不断呼吸的肺上面的伤口,跳动的心脏和不断收缩和扩张的动脉脉壁等,这些都是外科手术中的特殊挑战。
为了解决这些问题,生物医学工程师开发了一系列外科密封剂,可以黏合组织以阻止渗漏。
“目前可用的密封剂并不适合大多数手术的缝合过程中使用,因为它们缺乏弹性,不符合组织粘附和强度的需求。而我们所做的事情,就是使用我们在再生医学创建材料方面的专业知识,来制作一种可以在外科中使用的可以随着机体呼吸而“呼吸”的黏合胶水。我们同临床医生和生物工程师进行多学科的合作,为解决这个问题创造一个完美的解决方案。”哈佛大学生物启发工程学院Wyss研究所副教授Ali Khademhosseini博士说道。
最近在《科学转化医学》杂志上发表的一篇由Wyss研究所的Khademhosseini和东北大学的Nasim Annabi博士领导的研究小组,为有效修复机械性的身体部位的创伤提出了一个强大的解决方案,该研究团队还包括波士顿贝斯以色列女执事医疗中心(BIDMC)和澳大利亚悉尼大学的研究人员。
研究人员Khademhosseini说道:“基于人体中的弹性蛋白构成可以构成一种新的黏合剂,(弹性蛋白质存在于所有弹性组织如动脉壁,皮肤和肺中),这种黏合剂可以通过光化学来调节,从而可以有效地密封大鼠动脉和肺部的切口,修复猪肺部的伤口,并且实现全部缝合或无缝黏合!”
Khademhosseini是哈佛麻省理工学院卫生科学和技术部和布里格姆妇女医院的教授,东北大学化学系助理教授,哈佛麻省理工学院健康科学与技术部讲师。

MeTro直接作用于伤口,用光激活
2013年,这个灵感便诞生了。这个灵感来源于弹性蛋白纤维的天然的黏合能力。研究人员模仿身体的机制,学会了如何在大肠杆菌中产生大量的人类重组弹性蛋白,并使用被称为甲基丙烯酸酯的光交联试剂和紫外线的脉冲,在溶液中将它们交联不同的原丝胶蛋白从而创建一个多功能高弹性水凝胶,他们将这种多功能高弹性的水凝胶命名为MeTro。
而在这项研究中:MeTro可用于生成心脏细胞可以粘附的基质,并且可以作为组织构建体生长,用于心脏损伤的修复。
而最近的研究,研究人员进一步与BIDMC胸外科和介入性肺部科主任Sidhu Gangadharan D,肺癌专家George Cheng博士合作。
“与Sidhu和George谈论我们以前对MeTro的研究结果时,我们意识到肺损伤在外科来说尚且没有一个令人信服的解决方案,所以我们开始调查我们的材料是否可以作为肺和其他弹性组织的黏合剂,”Khademhosseini说道。
通过改变交联试剂的浓度,该团队生产了一系列具有不同弹性、粘性和黏合强度的MeTro水凝胶,然后在具有肺和血管损伤的动物模型中选择黏合效果最好的MeTro。这种方法是为了找到最接近组织自然弹性和强度的MeTro配方,即使在像血液这样的液体存在下也能很好地黏合到组织表面,而这对于其他黏合剂来说是很困难的一件事。
“我们可以肯定,这项研究的应用市场是极其广阔的。比如在紧急情况下,存在严重的内部伤口,如车祸和战区,这种黏合剂就可以很好的防止组织的进一步损坏。同时也可以改善医院的外科手术状况。我们已经研发了不同黏合强度和特性的黏合剂,解决了其他可用的黏合剂可能存在的问题。”研究人员说道。
目前该项研究在动物的应用中成果斐然。
在小鼠的研究中,这些新的MeTro凝胶可以无缝地封闭小鼠体内的切口,而在活的大鼠肺部的穿刺本可以使小鼠死亡,但是这项新的技术保证小鼠活了下来。而为了更加接近人体的状况,研究人员也在活体猪身上做出了相同的研究。该研究小组首先测试了MeTro是否也可以黏合猪不断活动的肺部。在猪吸气过程(肺膨胀)时,MeTro比临床可用的黏合线和缝合线表现出更好的密封性和黏合性。
而更重要的一点是:在体内实验中,MeTro可以永久性地密封严重的肺部空气和血液渗漏,不需要使用缝合针或缝线来进行二次修补!
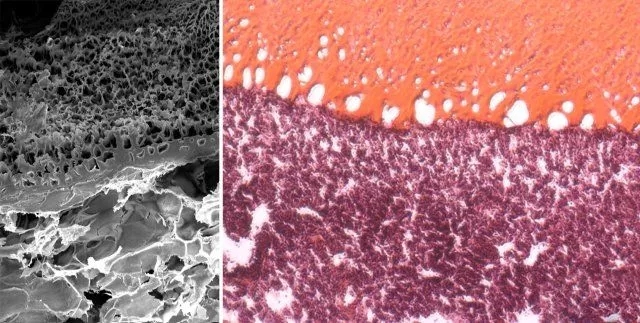
电子显微镜扫描照片和组织学染色切片:一个受伤的肺被一种MeTro修复,
连接紧密,密封性强
“MeTro水凝剂是一件伟大的艺术品。她的美丽之处在于:一旦与组织表面接触,就会凝固成凝胶状而不会消失,然后通过不断的固化,进一步保持稳定的状态,这使得密封剂可以被非常准确地放置在我们需要的部位上,并且与组织表面上的结构紧密结合并互锁,从而保持绝佳的密封性。“Khademhosseini说道。
“这项研究是人类生物学可以重新设计的一个很好的例子,通过不同的方式对黏合剂进行调整,以创造出一个令人惊讶的可以被广泛接受的解决方案,以适应在不同创伤情况下的患者。”Wyss研究所创始总监,医学博士,Donald Ingber博士说道。
原始出处:
Annabi N, Zhang YN, Assmann A,et al.Engineering a highly elastic human protein-based sealant for surgical applications.Sci Transl Med. 2017 Oct 4;9(410). pii: eaai7466. doi: 10.1126/scitranslmed.aai7466.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TRA#
59
#Transl#
49
#血管壁#
106
#动脉血#
75
#Med#
63
学习
106
学习了.谢谢
0