Intens Care Med:重症监护患者精神健康相关的生活质量与谵妄相关
2022-08-31 MedSci原创 MedSci原创
研究人员发现在ICU住院期间发生谵妄的ICU幸存者在入院前的精神健康相关生活质量明显较差,出院后一年的精神健康相关生活质量也显著下降。
重症监护病房(ICU)内谵妄发生在60-80%的机械通气患者和20-40%的非机械通气患者中。谵妄也被称为“意识障碍和基线认知的改变”,是一种全球性的认知障碍。谵妄被认为是ICU患者发病率和死亡率的独立预测因素。再者,ICU中谵妄的持续时间与长期认知障碍的发展有关。ICU住院期间的谵妄可能与病前精神疾病有关。
此外,ICU住院期间谵妄也可能对长期健康相关生活质量产生负面影响。

近日,危重病医学领域权威杂志Intensive Care Medicine上发表了一篇研究文章,该研究的目的是探讨ICU患者发生谵妄是否与发病前的精神生活质量相关,并影响ICU患者住院后的长期精神生活质量。
研究人员对1021名在外科ICU住院超过48小时的患者进行了一项前瞻性队列研究。研究人员采用Short-form-12量表评估了受试者入住ICU前、出院时、出院后3个月、6个月和12个月的身心生活质量。该研究的数据分析采用混合模型和逻辑回归模型的方法。
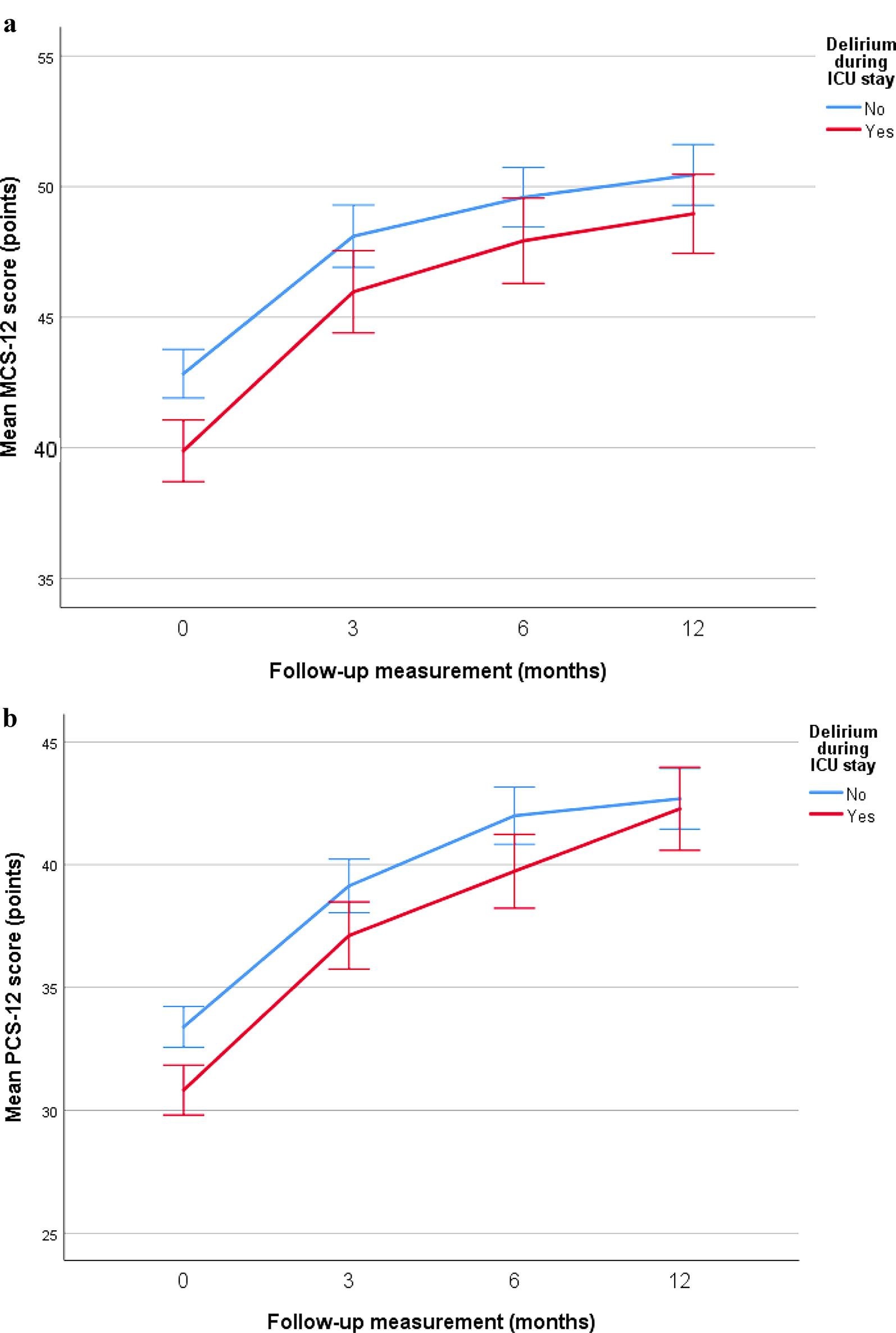
研究人员发现在ICU住院期间发生谵妄的患者报告的入院前精神生活质量低于未发生谵妄的患者(p<0.001)。此外,在ICU住院期间发生谵妄的患者与未发生谵妄的患者相比,随着时间的推移精神生活质量显著下降(p=0.035)。
在这项大型随访研究中,研究人员发现在ICU住院期间发生谵妄的ICU幸存者在入院前的精神健康相关生活质量明显较差,出院后一年的精神健康相关生活质量也显著下降。
原始出处:
José G. M. Hofhuis.et al.Mental health-related quality of life is related to delirium in intensive care patients.Intensive Care Medicine.2022.https://www.esicm.org/icm-search/?id=doi:10.1007/s00134-022-06841-8#article
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TENS#
71
#重症监护患者#
58
#监护#
62
#Med#
63