JAMA:PCI术后1年,还需要继续双抗血小板治疗吗?
2016-04-11 Mechront 译 MedSci原创
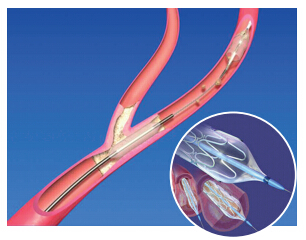
经皮冠状动脉介入术(PCI)后进行双重抗血小板治疗可减少缺血性风险,但会增加出血风险。研究者进行了一项试验,建立一个临床决策工具,以识别PCI术后1年持续使用噻吩并吡啶类抗血小板药物的优劣。该研究纳入了11个国家的11 648名患者(DAPT 研究),根据PCI术后12-30个月的缺血和出血风险建立预测规则,再经过8136名患者进行验证(PROTECT)。先进行长达12个月的噻吩并吡啶+阿司匹林治
经皮冠状动脉介入术(PCI)后进行双重抗血小板治疗可减少缺血性风险,但会增加出血风险。研究者进行了一项试验,建立一个临床决策工具,以识别PCI术后1年持续使用噻吩并吡啶类抗血小板药物的优劣。
该研究纳入了11个国家的11648名患者(DAPT 研究),根据PCI术后12-30个月的缺血和出血风险建立预测规则,再经过8136名患者进行验证(PROTECT)。
先进行长达12个月的噻吩并吡啶+阿司匹林治疗,再随机分为长达18个月的噻吩并吡啶+阿司匹林或安慰剂+阿司匹林。以PCI术后12-30个月缺血(心肌梗死(MI)或支架内血栓形成)和出血事件(中度或重度)作为主要终点。
数据显示,DAPT研究的患者其平均年龄为61.3岁,女性占25.1%,缺血和出血事件分别为348名(3.0%)和215名(1.8%)患者。推导队列模型预测缺血和出血的c统计分别为0.70和0.68。当前MI、前次MI或PCI、糖尿病、支架直径小于3mm、吸烟和紫杉醇洗脱支架时,预测值加1分;充血性心力衰竭、低射血分数和静脉移植干预史,则预测值加2分;年龄≥65岁,但<75岁,预测值-1分;≥75岁,预测值-2分。
对得分较高的患者(≥2分,n = 5917)继续进行噻吩并吡啶治疗,与安慰剂组相比,可减少缺血事件发生率(2.7% vs 5.7%; RD, −3.0% [95% CI, −4.1% to −2.0%], P < .001),与对得分较低的患者(<2分,n = 5731)相比,缺血事件发生率也下降了(1.7% vs 2.3%; RD, −0.7% [95% CI, −1.4% to 0.09%], P = .07; 交互作用P < .001)。
相反,对得分较高的患者(1.8% vs 1.4%; RD, 0.4% [95% CI, −0.3% to 1.0%], P = .26)继续进行噻吩并吡啶治疗,与对得分较低的患者(3.0% vs 1.4%; RD, 1.5% [95% CI, 0.8% to 2.3%], P < .001; 交互作用 P = .02)相比,会小幅度增加出血风险。
验证队列(PROTECT)的患者平均年龄62岁,其中女性占23.7%,缺血和出血事件分别为79名(1.0%)和37名(0.5%)名患者,缺血和出血的c统计均为0.64。此队列中,得分高的患者(n = 2848)与得分低的患者相比,缺血事件风险增加,出血风险两组间没有显著差异。
数据表明,对PCI术后1年不持续出现出血或缺血的患者而言,双抗血小板治疗对晚期缺血和出血风险的预测规则具有适当的准确性,无论是推导队列还是验证队列,在未来还需要更多的前瞻性研究,评估患者护理等对其潜在的影响。
原始出处:
Robert W. Yeh, MD, MSc; Eric A. Secemsky, MD, MSc,et al.Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year After Percutaneous Coronary Intervention.JAMA. Published online March 29, 2016. doi:10.1001/jama.2016.3775
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PCI术#
82
太高深'看不太明白
153
学习了,好文章
131
看不太明白
164
高大上的文章
155
值得学习
186
#PCI术后#
81
#双抗#
84