骨质疏松症基层合理用药指南,3分钟get要点!
2021-07-05 rayms 梅斯医学整理
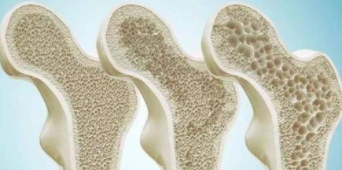
骨质疏松症是一种以骨量低、骨组织微结构损 坏为表现,导致骨脆性增加、易发生骨折为特征的全身性代谢性骨病 。
骨质疏松症是一种以骨量低、骨组织微结构损 坏为表现,导致骨脆性增加、易发生骨折为特征的全身性代谢性骨病 。骨质疏松症可发生于任何年龄,但多见于绝经后女性和老年男性。骨质疏松 症按病因分为原发性和继发性两大类,2021年中华医学会临床药学分会发布了《骨质疏松症基层合理用药》指南,主要针对原发性骨质疏松症。

一,药物治疗原则
(一)基本骨营养补充
抗骨质疏松症的治疗应强调在充足钙与维生素D营养补充的基础上,钙和维生素D的使用应贯 穿于整个骨质疏松治疗过程,与抑制骨吸收药和促 进骨形成药合用可提高骨密度,预防骨折风险。
(二)抑制骨吸收
破骨细胞骨吸收功能异常活跃会引起骨量丢 失过多,从而导致骨折风险。抑制骨吸收药通过减 少破骨细胞的生成或减少破骨细胞活性来抑制骨 吸收,对于快速骨丢失的严重骨质疏松症患者可使 用该类药物进行治疗。
目前抑制骨吸收药主要有双磷酸盐如阿仑膦 酸钠、唑来膦酸和利塞膦酸钠,选择性雌激素受 体调节药如雷洛昔酚 ,以及降钙素如鲑降钙素和 依降钙素等,它们对预防和或治疗骨质疏松症有效。
(三)促进骨形成
骨形成和骨吸收的动态平衡维持正常骨骼结 构和骨密度。当骨形成的量或速度低于骨吸收时, 就会发生骨质疏松。特立帕肽能促进成骨祖细胞 增生分化,直接抑制成骨细胞凋亡,延长成骨作用 时间,促进衬里细胞向成骨细胞转化及刺激成骨细 胞产生 IGF‑1和转化生长因子发挥其骨合成效应, 在促进骨形成方面有明确的疗效。
(四)其他机制类
该类药物能减慢骨重建,兼具抑制骨吸收和刺 激成骨细胞生长作用,如锶盐雷奈酸锶和异黄酮 衍生物依普黄酮 。
(五)抗骨质疏松药物的选择
对低中度骨折风险者,如相对年轻的绝经后妇 女,骨密度水平较低但无骨折史的患者,首选口服 药物如阿仑膦酸钠治疗。对口服不能耐受、依从性 欠佳及高骨折风险者,如多发椎体骨折或髋部骨折的老年患者、骨密度水平极低的患者,可考虑使用 注射剂如唑来膦酸、特立帕肽治疗。对于仅存在椎 体骨折高风险,而髋部和非椎体骨折风险不高的患 者,可考虑选用雌激素或选择性雌激素受体调节药 如雷洛昔芬治疗。新发骨折伴疼痛的患者,可考虑 短期使用降钙素治疗。
(六)抗骨质疏松药物的疗程
抗骨质疏松症药物疗程应个体化,所有治疗应 至少持续1年,建议静脉双膦酸盐治疗3年,口服双 膦酸盐治疗 5 年,疗程结束后对骨折风险进行评 估,如为低风险,可考虑实施药物假期;如骨折风险 仍高,可以继续使用双膦酸盐或换用其他抗骨质疏 松症药物。特立帕肽疗程为18~24个月,降钙素 连续使用时间一般不超过3个月。
pixabay
二,治疗药物
(一)阿法骨化醇
1,药品分类:骨营养补充药。
2,用药目的:用于提高骨密度。
3,禁忌证:禁用于对维生素 D 及其类似物过 敏、高钙血症、有维生素D中毒征象者。
4,不良反应及处理:小剂量单独使用(<1.0 μg/d) 一般无不良反应,长期大剂量用药或与钙剂合用可 能会引起高钙血症和高钙尿症,建议定期检查患者 血钙和尿钙水平。
5,药物相互作用:与钙剂合用可能会引起血钙 升高;与大剂量磷剂合用可诱发高磷血症;与噻嗪 类利尿剂合用有发生高钙血症的危险;与洋地黄毒 苷类药物合用若出现高钙血症易诱发心律失常;与巴比妥类药物合用可加速活性维生素 D 代谢物在 肝内代谢,降低本品药效;与考来烯胺或含铝抗酸 药合用可减少本药吸收。
(二)碳酸钙(或碳酸钙+维生素D3 )
1,药品分类:骨营养补充药。
2,用药目的:用于治疗钙缺乏症。
3,禁忌证:禁用于高钙血症、高钙尿症、含钙肾 结石或肾结石病史患者。
4,不良反应及处理:常见的不良反应有嗳气和 便秘,一般无需停药。
5,药物相互作用:与洋地黄毒苷类药物合用可 能出现高钙血症,易诱发心律失常;大量饮用含酒 精和咖啡因的饮料以及大量吸烟会抑制钙的吸收; 大量进食富含纤维素的食物会抑制钙的吸收;与四 环素和喹诺酮类抗菌药物合用可减少它们的吸收; 与维生素D、避孕药、雌激素合用能增加钙的吸收; 与含铝的抗酸药合用会使铝的吸收增多;与噻嗪类 利尿药合用时易发生高钙血症。
(三)骨化三醇
1, 药品分类:骨营养补充药。
2,用药目的:用于提高骨密度。
3, 禁忌证:禁用于对维生素 D 及其类似物过 敏、与高血钙有关的疾病、有维生素D中毒征象者。
4,不良反应及处理:不良反应发生率低(< 0.001 %),长期大剂量用药可能会引起高血钙综合 征或钙中毒,建议定期检查患者血钙或尿钙水平。 偶见的急性症状包括食欲减退、头痛、呕吐、腹痛和便秘,一般不需要停止治疗。
5,药物相互作用:与噻嗪类利尿剂合用会增加 高钙血症的危险;与洋地黄毒苷类药物合用可能出 现高钙血症,易诱发心律失常;与含镁药物(如抗酸 药)合用可能导致高镁血症;与大剂量磷剂合用可 诱发高磷血症;激素可能拮抗骨化三醇对钙的促吸 收作用;胆汁酸螯合剂(包括消胆胺和司维拉姆)可 能减少骨化三醇在肠道的吸收。
(四)阿仑膦酸钠
1,药品分类:抑制骨吸收药。
2,用药目的:用于预防骨质疏松症引起的骨折。
3,禁忌证:禁用于有食管动力障碍如食管迟缓 不能、食管狭窄者,30 min 内难以坚持站立或端坐 位者,对本品任何成分过敏者。
4,不良反应及处理:耐受性良好,少数患者可 见腹痛、腹泻、恶心、便秘、消化不良等,不良反应通 常轻微,一般不需要停止治疗。
5,药物相互作用:与抗酸药物或导泻剂合用会 影响阿仑膦酸钠吸收;与氨基糖苷类合用会诱发低 钙血症。
(五)唑来膦酸
1,药品分类:抑制骨吸收药。
2,用药目的:用于预防骨质疏松症引起的骨折。
3,禁忌证:禁用于对唑来膦酸或其他双膦酸盐 过敏者,严重肾功能不全患者,妊娠期和哺乳期 妇女。
4,不良反应及处理:最常见的不良反应为发 热,其他常见的有流感样症状如寒战、疲劳、无力和疼痛,骨骼肌肉疼痛如肌痛、关节痛、骨痛和背痛, 但其不良反应多为轻度和一过性的,多数情况下无 需特殊处理,会在 24~48 h内自动消退。
5,药物相互作用:与显著影响肾功能的药物如 氨基糖苷类或利尿剂合用可能会诱发低钙血症。
(六)利塞膦酸钠
1,药品分类:抑制骨吸收药。
2,用药目的:用于治疗和预防绝经后妇女的骨 质疏松症。
3,禁忌证:禁用于对利塞膦酸过敏者,低钙血 症患者,30 min 内难以坚持站立或端坐位者,哺乳 期妇女。
4,不良反应及处理:常见不良反应有消化系统 不良反应如吞咽困难、食道炎、食道或胃溃疡和流 感样综合征如头痛、头晕、皮疹、关节痛等。
5,药物相互作用:与钙剂、抗酸剂以及含二价 阳离子的口服制剂同服会影响吸收。
(七)雷洛昔芬
1,药品分类:抑制骨吸收药。
2,用药目的:用于治疗和预防绝经后妇女的骨 质疏松症。
3,禁忌证:禁用于妊娠期妇女,静脉血栓栓塞 性疾病者(包括深静脉血栓、肺栓塞和视网膜静脉 血栓者),对雷洛昔芬或片剂中所含的任何赋形剂 成分过敏者,肝功能减退包括胆汁瘀积,严重肾功能减退者,难以解释的子宫出血者,有子宫内膜癌 症状和体征者。
4,不良反应及处理:常见不良反应有潮热出 汗、腿部痉挛,绝大多数不良反应无需停止治疗;严 重不良反应有深静脉血栓形成、静脉血栓栓塞、脑 血管意外、肺栓塞。
5,药物相互作用:与消胆胺(或其他阴离子交 换树脂)同时服用可显著减低雷洛昔芬的吸收和肠 肝循环;雷洛昔芬可轻度增加激素结合球蛋白的浓度。
(八)鲑降钙素
1,药品分类:抑制骨吸收药。
2,用药目的:用于降低破骨细胞活性和数目, 直接抑制骨吸收,减慢骨转换。
3,禁忌证:禁用于对鲑降钙素或者本制品任何 成分敏感者。
4,不良反应及处理:可出现恶心、呕吐、头晕、 轻度的面部潮红伴发热感,这些反应常常自发性消 退,仅在极少数患者需暂时性减少剂量。
5,药物相互作用:降钙素与锂合用可能导致血 浆中锂浓度下降。
(九)依降钙素
1, 药品分类:抑制骨吸收药。
2,用药目的:用于治疗骨质疏松症及骨质疏松 引起的疼痛。
3,禁忌证:禁用于对依降钙素成分有过敏史的 患者。
4,不良反应及处理:参考鲑降钙素。
5,药物相互作用:与二膦酸盐类骨吸收抑制剂 合用可能出现低钙血症。
(十)特立帕肽
1,药品分类:促进骨形成药。
2,用药目的:用于降低骨折高发风险的绝经后 妇女椎骨和非椎骨骨折风险。
3,禁忌证:禁用于对特立帕肽或其任何赋形剂 过敏者,妊娠及哺乳期妇女,高钙血症患者,严重肾 功能不全患者,除原发性骨质疏松和糖皮质激素诱 导的骨质疏松以外的其他骨骼代谢疾病(包括甲状 旁腺功能亢进和Paget病),不明原因的碱性磷酸酶 升高者,之前接受过外照射或骨骼植入放射性治疗 的患者。
4,不良反应:最常见的不良反应有恶心、肢体 疼痛、头痛和头晕。
5,药物相互作用:特立帕肽能瞬时提高血钙水 平,高血钙可能导致患者洋地黄中毒,因此使用洋 地黄的患者应慎用特立帕肽。
(十一)雷奈酸锶
1,药品分类:抑制骨吸收和促进骨形成双重作用药物。
2,用药目的:用于治疗绝经后骨质疏松症以降 低椎体和髋部骨折的危险性。
3,禁忌证:禁用于对本药成分和任何赋形剂成 分过敏者。
4,不良反应及处理:常见不良事件有恶心和腹 泻,通常程度轻微并且短暂;严重不良反应如静脉 血栓,严重的超敏反应综合征,特别是伴有嗜酸粒 细胞增多和全身症状的药物疹,需要停止使用雷奈 酸锶并开始皮质激素治疗,通常结果良好。
5,药物相互作用:食物、牛奶和牛奶制品,以及 含有钙的药品降低雷奈酸锶生物利用度 60%~ 70%,需间隔2 h服用;氢氧化铝和氢氧化镁在服用 雷奈酸锶之前 2 h服用或同时服用,雷奈酸锶的吸 收稍有降低;与四环素和喹诺酮类抗菌药物合用可 减少它们的吸收。
(十二)依普黄酮
1,药品分类:抑制骨吸收和促进骨形成双重作 用药物。
2,用药目的:用于改善骨质疏松症的骨量 减少。
3,禁忌证:禁用于对依普黄酮过敏者,低钙血 症患者。 4. 不良反应:常见的不良反应有胃纳减退、恶 心、呕吐、腹痛、腹胀。
4,不良反应:常见的不良反应有胃纳减退、恶 心、呕吐、腹痛、腹胀。
5,药物相互作用:与雌激素、茶碱和香豆素类 抗凝剂合用时,会增强它们的作用,应慎用。
原始出处
中华医学会 中华医学会临床药学分会 中华医学会杂志社 中华医学会全科医学分会 中华医学会《中华全科医师杂志》编辑委员会 基层医疗卫生机构合理用药指南编写专家组.骨质疏松症基层合理用药指南.中华全科医师杂志 2021 年5 月第 20 卷第 5 期 Chin J Gen Pract, May 2021, Vol. 20, No. 5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












已学习
94
学习了
108
学习下
109
学习
119
#合理用药#
125
#骨质#
78
厉害了。。。
112
学习了。
0