Nat Commun:血液凝固机制的发现对新的抗血栓药物研发有了新进展
2021-06-08 Viho MedSci原创
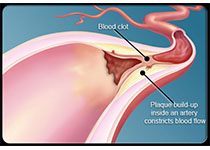
导致血栓形成的三大类因素--血液、血管和血流之间的相互作用。。研究人员首次确定了血管性血友病因子(VWF)的特殊机制--一种必需的凝血蛋白,它主要由血管内衬的内皮细胞分泌,它通过感知和响应血液剪切流量
导致血栓形成的三大类因素--血液、血管和血流之间的相互作用。。研究人员首次确定了血管性血友病因子(VWF)的特殊机制--一种必需的凝血蛋白,它主要由血管内衬的内皮细胞分泌,它通过感知和响应血液剪切流量的变化,使其能够与血小板结合并启动凝血。严重地介导止血、血栓形成和血栓炎症。
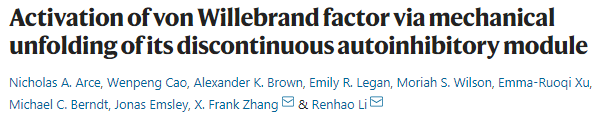
最近在Nature Communications发表的文章中,研究人员首次确定了vWF的特定结构元素,使其能够与血小板结合并启动凝血。研究小组发现,这个特殊的单位,他们称之为不连续的自动抑制模块,或称AIM,是新药开发的主要场所。血管性假血友病因子的激活是通过机械地展开其不连续的自抑制模块来实现的。
在正常、健康的循环条件下,血管性血友病因子(VWF)自我维持。巨大而神秘的糖蛋白在血液中流动,紧紧地包裹在一起,其反应部位未暴露。但当大量出血发生时,它就会产生作用,启动凝血过程。
当它正常工作时,vWF有助于止血和挽救生命。在这项研究中,研究小组确定了一个结构元件-AIM,位于vWF的一部分,称为A1结构域,负责与血小板结合。AIM是机械稳定的纳米体,其中包括caplacizumab,这是迄今为止FDA批准的唯一抗血栓药物,以VWF为目标。它的工作原理是绑定到vWF并阻止它与血小板结合。在低剪切条件下,血浆VWF受自身抑制,不与血小板GPIB-IX复合物的主要亚基糖蛋白(GP)Ibα结合。然而,当vwf暴露于高剪切状态或在流动中被固定时,它会经历张力,并随后暴露其a1结构域,以便与gpibα和血小板结合。
AIM模块允许vWF分子在正常循环血液中保持非反应性,并在出血时立即激活vWF。”在研究中,科学家们发现caplacizumab通过结合vWF的AIM区域和提高力阈值来机械地去除vWF的自身抑制结构,为开发针对AIM结构的抗血栓药物开辟了一条新的途径。
vWF的一个基本特征是它在循环中大部分时间对血小板没有反应。然而,在出血部位,vWF几乎可以立即被激活,以实现血小板粘附和凝血凝块的形成。
不连续AIM的协同展开
在正常的循环血液中,AIM包裹在A1周围,阻止A1与血小板的相互作用。然而,在结合部位,血流模式的改变会导致足够的水动力来拉伸AIM并将其从A1中拉开,从而使A1能够抓取血小板到出血部位。”不连续的AIM确实抵抗拉力,并协同展开超过一定的力阈值暴露A1。实验数据表明,在病理相关的条件下,AIM的破坏与与GPIBα的A1亲和力的增加有关。最后,AIM可以被一种新开发的抗血栓药物有效地靶向。
这个抑制模块在vWF中发挥如此重要的作用,它不仅控制vWF激活血小板相互作用,而且在触发某些类型的血管性血友病(一种遗传性出血疾病,影响到1%的人类人口)中发挥作用。了解VWF的机制,是阐明血栓性疾病的病理生理,发展安全的抗血栓治疗药物的关键。
文章参考:Nicholas A. Arce, Wenpeng Cao, Alexander K. Brown, Emily R. Legan, Moriah S. Wilson, Emma-Ruoqi Xu, Michael C. Berndt, Jonas Emsley, X. Frank Zhang, Renhao Li. Activation of von Willebrand factor via mechanical unfolding of its discontinuous autoinhibitory module. Nature Communications, 2021; 12 (1) DOI: 10.1038/s41467-021-22634-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#COMMUN#
81
#Nat#
111
#抗血栓药#
76
#抗血栓药物#
122
#研发#
117
#药物研发#
119
#抗血栓#
82
谢谢
148
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
172
恕我直言,写的一点不通顺,明显机器直接翻译的
126