PNAS:抗血管生成药物可显著改善肺结核的治疗
2015-02-03 MedSci MedSci原创
使用相同的改善癌症治疗效果的抗血管生成药物有助于克服肺结核(TB)治疗过程中持续的困难。通过了解应用于肿瘤生物学三年的工作中,我们首次证明结核肉芽肿有异常血管网,解释了先前NIAID共同作者的观察。PNAS早期版报告的共同作者博士Rakesh K. Jain说,我们的研究结果显示贝伐单抗——FDA批准的现在广泛应用于肿瘤和眼疾病的药物——可以矫正肉芽肿血管,提高小分子传递,并显示这种药物与抗结核药
使用相同的改善癌症治疗效果的抗血管生成药物有助于克服肺结核(TB)治疗过程中持续的困难。通过了解应用于肿瘤生物学三年的工作中,我们首次证明结核肉芽肿有异常血管网,解释了先前NIAID共同作者的观察。PNAS早期版报告的共同作者博士Rakesh K. Jain说,我们的研究结果显示贝伐单抗——FDA批准的现在广泛应用于肿瘤和眼疾病的药物——可以矫正肉芽肿血管,提高小分子传递,并显示这种药物与抗结核药物联合使用可提高结核病的治疗,减少抗生素耐药性日益严重的问题。
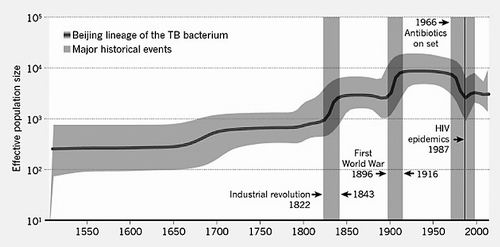
全世界三分之一可能是细菌感染引起的肺结核,大多数感染者不发病。因削弱了免疫系统,如HIV感染,化疗,或其他原因可以导致肺结核的发病,其中细菌增殖可使肺组织和其他器官的遭到攻击。治疗结核病涉及多种抗生素的药物,日益严重的问题是用来治疗肺结核细菌耐药菌株的出现,有对十种药物都有抵抗,这导致全世界每年几乎2百万病人的因结核病死亡。
最近的研究探讨了人类和动物的肺结核肉芽肿的结构特点,并对PNAS早期版报告研究共同作者克利夫顿巴里三世博士和其他人观察到的抗结核药物渗透到病变组织的能力差别很大,很少能在死亡细胞的中央区域内达到高浓度。另一方面对肉芽肿的环境包括低水平氧,可以抑制免疫细胞的作用已得到证实。
因为在目前的研究中,研究小组发现了在兔肺结核与肿瘤之间肉芽肿血管网络的几个相似性——包括强有力的血管生成因子VEGF表达升高,这也是从人类肉芽肿患者中发现的;缺乏支持细胞,血管壁结构异常;在病变血管的分布极不均衡。静脉注射荧光染料分子在大小上与常用的抗结核药物相似,并显示功能异常的肉芽肿血管限制了很少或没有到达中央区域病灶的染料的渗透。
贝伐单抗是一种阻断VEGF的抗体,对肉芽肿血管在结构上进行改善——如血管直径增加,增加更多的支持细胞,以及去除无效的、不成熟的血管,这些结构化的血管也得到功能上的改进。血管生成药物用于癌症的治疗,这些影响是暂时的,持续不到一个星期,但研究人员希望周期性的贝伐单抗给药可改善抗结核药物的治疗效果。除了减少结核病治疗的周期,消除物理障碍,保持所有给予药物到达细菌内肉芽肿从而减少细菌耐药性的发展。
“不像其他研究者对结核病的研究,我们不寻求发现对抗细菌耐药性的新途径,而我们正在努力克服对这些血管异常引起的生理性抵抗的治疗,”哈佛医学院肿瘤生物学教授Jain指出。“由于我们使用的是FDA批准的药物,我们的工作必须具有临床应用的潜力。”
原始出处:
Meenal Datta, Laura E. Via, Walid S. Kamoun, Chong Liu, Wei Chen, Giorgio Seano, Danielle M. Weiner, Daniel Schimel, Kathleen England, John D. Martin, Xing Gao, Lei Xu, Clifton E. Barry Iii, and Rakesh K. Jain. Anti-vascular endothelial growth factor treatment normalizes tuberculosis granuloma vasculature and improves small molecule delivery. PNAS, January 2015
本文是MedSci原创,欢迎转发,转发请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抗血管生成药物#
146
#抗血管#
70
#PNAS#
130
激素与抗结核药同时应用可提高结核病的治愈率
167
药物相互作用越来越多!
199
#结核#
123
#抗血管生成#
63