家族性高胆固醇血症诊断率低,出现黄色脂肪瘤须警惕
2017-06-01 屠俊 澎湃新闻
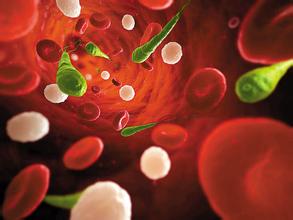
近日,据台湾媒体报道,台北市一名28岁女性,血中胆固醇数值高达一般人的七八倍,心脏血管、冠状动脉到处都塞住,尽管接受了多次的扩张术、放过支架,血管依旧狭窄阻塞,开完刀不久就因心律不整过世,只因罹患家族性高胆固醇血症(FH)。高胆固醇血症(FH)是一种罕见的常染色体显性遗传性疾病,有家族性的特征,主要病因为基因突变,涉及的基因主要有LDL受体基因、ApoB基因以及PCSK9基因突变,其主要临床表现为
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#诊断率#
85
#高胆固醇血症#
70
#脂肪瘤#
81
#家族性#
0
好好文章学习了
75
学习
77
需重视,谢谢
73
好文章学习了
85