氟喹诺酮类 (FQ) 是一类广泛使用的抗生素,对革兰氏阴性菌和革兰氏阳性菌均具有广谱活性。虽然FQ的耐受性通常良好,但 FQ的使用与多种器官系统相关的不良反应有关。
报告表明,与口服FQ相关的主动脉和二尖瓣关闭不全的风险增加,导致欧洲药品管理局(EMA)发布了安全警告。但是该现象尚未经过验证。
采用丹麦的行政登记,Emanuel等研究人员在2005年至2018年期间的全国性个人队列中进行了嵌套病例对照研究。病例定义为首次发生主动脉瓣或二尖瓣反流的患者。暴露因素为口服FQ。采用Cox回归模型评估风险比(HR)和95%置信区间(95%CI),以评估FQ使用和偶发性瓣膜反流的相关性。
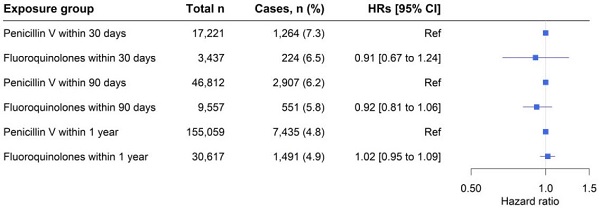
FQ暴露与主动脉瓣或二尖瓣反流率的相关性
共纳入了38370例偶发性瓣膜反流病例和1115100例匹配的对照。与青霉素V使用者相比,FQ暴露与主动脉瓣或二尖瓣反流率增加显著相关(HR 1.02,95%CI 0.95-1.09)。对FQ累积限定剂量(cDDD)的研究得到了类似的结果,但FQ暴露量增加与瓣膜反流之间无显著关联(与cDDD 1-5相比,cDDD>10的HR 1.08, 95%CI 0.95-1.23)。这些结果在多项分析中是一致的,包括一组高血压患者和使用瓣膜手术干预的病例。
总而言之,这项全国性的病例对照研究表明,FQ暴露与瓣膜反流率增加没有显著相关性。该研究结果不支持FQ暴露与发生瓣膜反流之间可能存在因果关系。
原始出处:
Strange Jarl Emanuel,Holt Anders,Blanche Paul et al. Oral fluoroquinolones and risk of aortic or mitral regurgitation: a nationwide nested case-control study.[J] .Eur Heart J, 2021, https://doi.org/10.1093/eurheartj/ehab374
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#喹诺酮#
92
#氟喹诺酮类抗生素#
84
#ART#
74
#氟喹诺酮#
83
#HEART#
83
#反流#
112
#瓣膜#
70
氟喹诺酮类抗生素还增加主动脉瘤和主动脉夹层的风险。
123
学习
110
这个题目闻所未闻
126