Blood:阻断CTLA-4或可成为对阻断PD-1耐受的cHL患者的新治疗方向
2019-10-14 MedSci MedSci原创
经典霍奇金淋巴瘤(cHL)是一种罕见的由非典型生发中心来源的B细胞(HRS细胞)构成的肿瘤;HRS细胞嵌在一个健壮但无效的炎症环境中。cHL肿瘤微环境(TME)被分割成富含PD-L1阳性HRS细胞和肿瘤相关巨噬细胞(TAMs)的“壁龛”,与PD-1阳性T细胞结合,通过PD-L1/PD-1信号通路抑制抗肿瘤免疫。虽然cHL对PD-1检查点阻断非常敏感,但大多数患者最终会复发,需要其他治疗方案。采用多
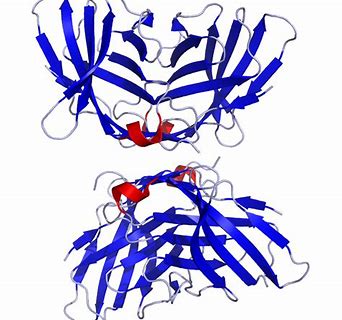
采用多重免疫荧光显微镜数字图像分析,研究人员发现与反应性淋巴组织相比,cHL高度富集非调节CTLA-4阳性T细胞,其数量甚至超过了PD-1和LAG-3阳性T细胞。此外,接触HRS细胞的T细胞中,CTLA-4阳性率远高于PD-1或LAG-3的阳性率高。
此外,研究人员进一步发现,HRS细胞和TAMs的一种亚型,对CTLA-4配体CD86呈阳性,而CTLA-4阳性和CD86阳性的T细胞和TAMs在75um HRS细胞壁龛内的占比也明显多于该区域以外的区域。重要的是,在经过包括PD-1阻断在内的多种治疗后,复发性cHL肿瘤中常存在CTLA-4阳性细胞和局部接触的HRS细胞。
综上所述,本研究表明CTLA-4:CD86相互作用是围绕HRS细胞的免疫优势壁龛的组成部分,并增加了对PD-1阻断难以治愈的cHL患者可能受益于CTLA-4阻断的可能性。
原始出处:
Sanjay S. Patel, et al.The microenvironmental niche in classic Hodgkin lymphoma is enriched for CTLA-4- positive T-cells that are PD-1-negative.blood.2019002206. https://doi.org/10.1182/blood.2019002206
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#cHL#
73
#阻断#
70
#CTLA-4#
60