Sci Rep:miR-107的缺乏促进了胰腺癌的发展
2017-08-07 MedSci MedSci原创
血浆中肿瘤抑制因子miR-107的减少与肿瘤进展有关,是治疗胰腺癌新型靶点。本研究探讨胰腺癌(PCa)患者肿瘤抑制微小RNA(miRNA)血浆水平的降低,以阐明其作为新生物标志物和治疗靶点的潜力。研究使用基于microRNA阵列的方法通过比较PCa患者和健康志愿者的血浆水平来选择候选者。选择六个下调的miRNA(miR-107,miR-126,miR-451,miR-145,miR-491-5p和
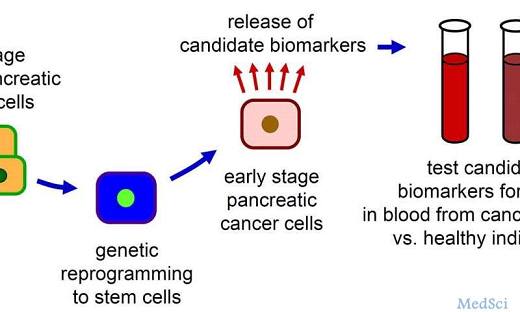
血浆中肿瘤抑制因子miR-107的减少与肿瘤进展有关,是治疗胰腺癌新型靶点。本研究探讨胰腺癌(PCa)患者肿瘤抑制微小RNA(miRNA)血浆水平的降低,以阐明其作为新生物标志物和治疗靶点的潜力。
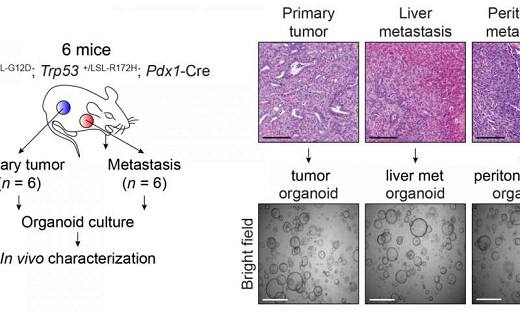
研究使用基于microRNA阵列的方法通过比较PCa患者和健康志愿者的血浆水平来选择候选者。选择六个下调的miRNA(miR-107,miR-126,miR-451,miR-145,miR-491-5p和miR-146b-5p)。使用100例PCa患者和80例健康志愿者的样本进行小规模和大规模分析显示,与健康志愿者相比,miR-107是PCa患者中最多的下调miRNA(P <0.0001;接受者操作特征曲线下面积,0.851)。低miR-107血浆水平与晚期T期,N期,和肝转移有关,是预测PCa患者预后不良的独立因素(P= 0.0424;风险比2.95)。
总之,该研究表明,miR-107在PCa细胞中的过表达通过产生p21诱导G1/S阻滞,并通过Notch2的转录调控抑制细胞增殖。在体内,miR-107血浆水平的恢复和维持显着抑制小鼠的肿瘤进展。血浆中肿瘤抑制因子miR-107的消耗与肿瘤进展和不良结局有关。血浆miR-107水平的恢复可能是PCa的新型抗癌治疗策略。
原始出处:
Taisuke Imamura, Shuhei Komatsu, et al., Depleted tumor suppressor miR-107 in plasma relates to tumor progression and is a novel therapeutic target in pancreatic cancer. Sci Rep. 2017; 7: 5708. Published online 2017 Jul 18. doi: 10.1038/s41598-017-06137-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#miR#
77
学习了谢谢分享!!
106
谢谢分享,学习了!
151
谢谢分享,学习了
91