ACCR年会:联合用药提高PARP抑制剂在耐药卵巢癌中的应答
2017-04-04 MedSci MedSci原创
来自Dana-Farber癌症研究所的科学家称,约三分之一的对PARP抑制剂无应答的卵巢癌患者接受激酶抑制剂治疗后,其肿瘤部分收缩。
来自Dana-Farber癌症研究所的科学家称,约三分之一的对PARP抑制剂无应答的卵巢癌患者接受激酶抑制剂治疗后,其肿瘤部分收缩。
2017年4月2日星期日下午3点,Panagiotis Konstantinopoulos博士在美国癌症研究协会(AACR)年会临床试验分论坛的大会报告中提到"当我们将这PARP抑制剂和激酶抑制剂联用时,我们获得了非常好的应答率--对铂类药物耐药的卵巢癌患者的应答率高达36%。"
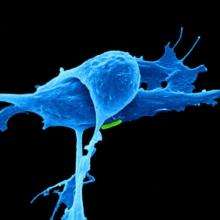
28例高级别浆液性卵巢癌患者在I期临床试验中接受了olaparib,一种PARP抑制剂,以及一种有效的PI3α抑制剂BYL719联合治疗。28例患者中有26例对铂类药物耐药。在这些患者中,对于PARA抑制剂本身的应答率低至4%,Dana-Farber的苏珊·史密斯女性癌症中心的医学肿瘤学家Konstantinopoulos说道。
在临床前研究中,添加PI3K抑制剂似乎使癌细胞对PARP抑制剂的作用敏感,这损害了肿瘤细胞的DNA修复能力。Konstantinopoulos说:"卵巢癌患者的中位持续应答时间为5.5个月左右,'这个应答持续时间对患者来说比较合适'"。 目前还有5例患者在接受治疗中。
Olaparib被批准用于治疗与BRCA基因缺陷相关的对铂类药物耐药的卵巢癌妇女。然而,在目前的试验中,无种系BRCA突变妇女的应答率为29%,而在非遗传性BRCA突变的患者中,应答率为33%。
总之,该组合药对的耐受性良好,据报道:仅四名患者因毒性大而停药。
Konstantinopoulos说:"联合疗法在无种系BRCA突变的耐药性卵巢癌患者中的疗效优于Olaparib单药治疗,值得进一步研究。"
原文出处:
此文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抑制剂#
61
#ACC#
59
#联合用药#
57
#PARP#
65