TUKYSA(tucatinib)在澳大利亚获得批准,用于治疗转移性HER2阳性乳腺癌
2020-08-12 Allan MedSci原创
TUKYSA是一种口服药物,是HER2蛋白的酪氨酸激酶抑制剂。
西雅图遗传公司今日宣布,澳大利亚监管机构已批准TUKYSA®(tucatinib)与曲妥珠单抗、卡培他滨联用,以治疗晚期不可切除或转移性HER2阳性乳腺癌患者,包括脑转移患者。澳大利亚与美国、瑞士、加拿大和新加坡一道组成了奥比斯计划(Project Orbis),奥比斯计划是美国食品药品监督管理局(FDA)肿瘤学卓越中心的一项举措,以促进国际监管机构同时审查抗肿瘤药物。4月份,TUKYSA成为奥比斯计划在美国批准的首个新药,目前正在欧盟接受审查。

西雅图遗传学执行总监Clay Siegall博士说:“奥比斯计划对TUKYSA的并发全球审查将使这种新型疗法快速进入市场,我们期待将TUKYSA带给世界各地的患者”。
该批准基于关键性试验HER2CLIMB(双盲安慰剂对照试验)的结果,该试验招募了612例先前曾分别接受过曲妥珠单抗、帕妥珠单抗等疗法治疗后复发的患者。研究结果于2019年12月发表在《新英格兰医学杂志》上。
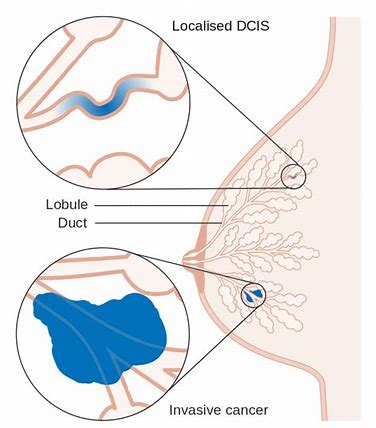
TUKYSA是一种口服药物,是HER2蛋白的酪氨酸激酶抑制剂。在体外试验中,TUKYSA抑制HER2和HER3的磷酸化,从而抑制下游MAPK和AKT信号传导以及细胞增殖,并在表达HER2的肿瘤细胞中显示出抗肿瘤活性。在体内试验中,TUKYSA抑制HER2阳性肿瘤的生长。TUKYSA和抗HER2抗体曲妥珠单抗的组合在体外和体内均显示出增强的抗肿瘤活性。在美国,TUKYSA与曲妥珠单抗和卡培他滨组合被批准用于晚期不可切除或转移性成年患者HER2阳性乳腺癌,包括患有脑转移患者。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#获得批准#
53
#HER2阳性#
62
#转移性#
65
#澳大利亚#
58
#Tucatinib#
54
广大乳癌患者**#乳腺癌#
181