盘点:近期前列腺癌相关研究进展一览
2017-02-19 MedSci MedSci原创
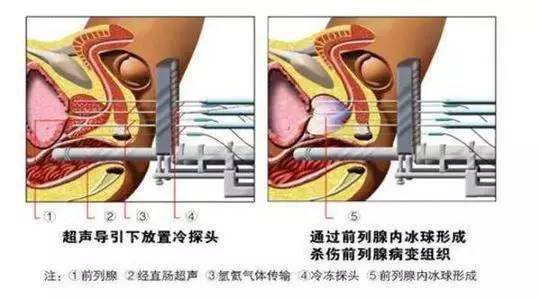
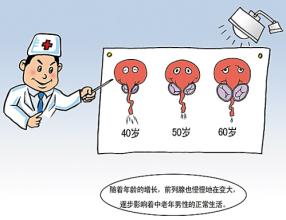
前列腺癌是欧美老年男性中发病率第一的恶性肿瘤,近年来在中国的发病率不断升高。大量数据表明,前列腺癌好发于中老年人,患者平均发病年龄在65岁以上。这里梅斯小编整理了近期关于前列腺癌的重要研究一览,与大家分享学习。【1】NEJM:抗雄激素联合放疗显著降低前列腺癌死亡率近期,权威杂志NEJM进行了一项研究。此项研究为1998年至2003年进行的双盲安慰剂对照试验,研究者们分配了760例经过淋巴结切除
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#期前列腺癌#
57
#相关研究#
72
#研究进展#
59
好资源
103
非常棒的文章,又学习了
97
小编辛苦了,感谢为我们准备了绝佳的精神晚餐,给点赞了!
91
好内容,认真学习
91
psa的筛查
90
归纳出的好东西!
65
前列腺癌为什么欧美国家老年男性发病率高
60