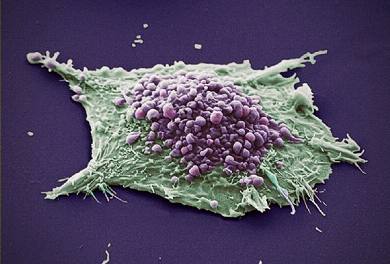
Ann Oncol:非小细胞肺癌的循环肿瘤细胞系的前瞻性研究
2017-07-26 MedSci MedSci原创
背景:曾几何时,晚期非小细胞肺癌(NSCLC)患者只能接受化疗。但是,其疗效已经到了一个瓶颈期,无法再进一步。可喜的是,随着人们对分子遗传学认识的不断增强,NSCLC 被细分为各种不同的分子亚型。本研究是第一个根据非小细胞肺癌(NSCLC)的分子亚型报告循环肿瘤细胞(CTC)的临床特征、数值性质和生物学特性。病人和方法:125例处于首次治疗阶段的IIIb-IV NSCLC患者被前瞻性招募到Cell
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
63
#Oncol#
63
#前瞻性研究#
57
#前瞻性#
0
好办法,希望能治理好。
96
#肿瘤细胞#
58
#细胞系#
66
#循环肿瘤细胞#
77
学习了
88
越来越多的发现,学习了
82