ASCO 2015:中国直肠癌研究FOWARC发现围手术期应用mFOLFOX6化疗方案可能改善DFS
2015-06-07 王迈 中国医学论坛报
由于结直肠癌在欧美国家乃至全球的高发病率和死亡率,该领域的研究和报告在每年的美国临床肿瘤学会(ASCO)年会上都是参会医生和媒体关注的焦点,而ASCO年会结直肠癌口头报告专场(oral session)也集中了这一领域全球最新、最好的一些研究。当地时间5月30日下午, 在ASCO 2015结直肠癌口头报告专场中,第一位走上讲台的是来自中国的学者——中山大学附属第六医院汪建平教授,他代表FOWA
由于结直肠癌在欧美国家乃至全球的高发病率和死亡率,该领域的研究和报告在每年的美国临床肿瘤学会(ASCO)年会上都是参会医生和媒体关注的焦点,而ASCO年会结直肠癌口头报告专场(oral session)也集中了这一领域全球最新、最好的一些研究。
当地时间5月30日下午, 在ASCO 2015结直肠癌口头报告专场中,第一位走上讲台的是来自中国的学者——中山大学附属第六医院汪建平教授,他代表FOWARC研究课题组进行了题为“mFOLFOX6联合或不联合放疗用于局部进展期直肠癌新辅助治疗的多中心随机对照研究:初步结果”的发言。(摘要号 3500)
“接地气”的研究设计
FOWARC是一项研究者发起的临床试验(IIT),探索了在围手术期应用mFOLFOX6化疗方案[奥沙利铂、四氢叶酸、5-氟尿嘧啶(5-FU)]是否可以改善局部进展期直肠癌(LARC)患者的无疾病生存(DFS)。

主要研究者(PI)汪建平教授在接受本报采访时告诉记者,FOWARC研究的设计是基于其团队对直肠癌新辅助治疗前期探索的结果——在2007-2010年间,由于标准治疗5-FU联合放疗的直肠癌新辅助治疗对远处控制不理想,国际上都试图探索把奥沙利铂加入到直肠癌的新辅助治疗,而他们也开始尝试在放疗同时使用全量全身治疗的化疗方案(FOLFOX),结果发现患者初步的耐受性及疗效都比较理想。因此,研究者萌生了扩大成大型临床研究的想法,以期比较在直肠癌新辅助治疗中全量FOLFOX化疗联合放疗与5-FU增敏放疗的疗效。
在研究设计讨论中,考虑到一些收治直肠癌患者的三甲医院并没有放疗设备——一个中国特有的因素,以及放疗相关毒性,研究者同时设计了一组新辅助治疗单纯使用FOLFOX全量化疗,之后根据病情需要决定术后是否加入放疗,这就形成了本研究的第3个“接地气”的分组。
“跻身”ASCO讲台的“初步”结果
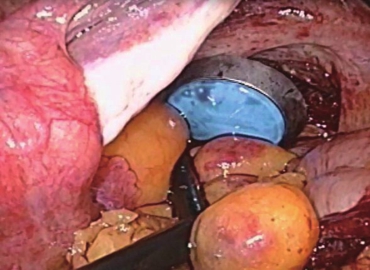
2011年1月至2015年2月间,这项多中心研究共纳入495例患者,随机进入对照组(5-FU单药化疗联合放疗)、FOLFOX-RT组(mFOLFOX6化疗联合放疗)以及FOLFOX组(单纯接受4~6周期的mFOLFOX6化疗,并根据需要接受术后放疗)。
本次ASCO年会上,汪建平教授报告了包括病理完全缓解(pCR)率在内的初步结果:对照组、FOLFOX-RT组、FOLFOX组的R0切除率分别为90.1%、88.2%和91.2%;pCR率分别为14.3%、28%和6.1%;各组分别有37.6%、57.4%和35.8%的患者实现了肿瘤显著降期(新辅助治疗后TNM分期降为0~Ⅰ期)。

据研究第一作者邓艳红教授介绍,主要终点DFS结果预计将于2年后公布。局部进展期直肠癌的治疗策略一直是结直肠癌领域的热点,而相关研究均会先报告pCR结果,这是此次跻身ASCO讲台的重要原因。
领导与协作:IIT推进的关键
谈及FOWARC研究执行中的体会,邓艳红教授表示,患者对新辅助治疗的接受度以及医生对研究的认可度,是研究推进的巨大障碍,“要有一个好的PI,和一群比较有协助精神的人,这是首要条件。”在中国,IIT研究能够坚持推进并不是件容易的事情,而FOWARC研究的步步推进与汪建平教授对整个研究项目的领导以及各研究中心的协调、协作密不可分。
现场专家点评
比利时鲁汶大学泰帕(Sabine Tejpar)教授:
这是一项设计非常平衡、数据呈现非常清晰的研究,我基本上能从你们的报告中找到我想了解的信息。
pCR作为直肠癌研究的替代终点,长期以来存在很多争议和质疑。因此对于FOWARC研究,继续随访等待数据成熟并产生更加“经典”的研究终点数据,以真正反映3组患者的预后,这是十分重要的。
另外,我认为3组的研究设计是极为聪明的,因为减少任何一个研究组可能都不会有如此的吸引力。仅从FOWARC目前的研究设计和数据来看,我个人非常看好这一研究的结果。
在临床实践中,有很多医生极其信赖FOLFOX研究,也有很多直肠癌领域的相关研究正在进行,所以,我认为,这些数据最终会有助于一些医生的临床决策。(注:Tejpar教授为国际结直肠癌分子分型领衔专家)
美国西北大学罗伯特H.卢里(Robert H. Lurie)综合癌症中心本森(Al B. Benson)教授:
我对这项研究的长期随访结果会非常感兴趣,因为尽管美国国立综合癌症网络(NCCN)指南建议术后患者应该接受FOLFOX化疗,但是在美国也有很多患者在新辅助放疗(5-FU增敏)及手术治疗后不再做化疗。这样的决定往往包含了患者和医生双方面的因素,尤其是那些新辅助治疗效果明显的患者。因此,大家非常关注把化疗提前的可能性,考虑这样的策略可能耐受性和接受度都更高。
对于肿瘤位置比较高的患者,也有研究者在探讨能否避免放疗。美国有在肿瘤位置距肛缘>5 cm的患者中,比较5-FU/放疗+手术+化疗与根据FOLFOX化疗效果决定术前是否进行放疗的研究。但是,对于低位肿瘤的患者,避免放疗的代价可能是高局部复发率(LRR),因此需要特别注意。
更进一步,我们现在还不清楚是否应该根据分期的不同,给予高位直肠癌患者不同的治疗策略。在结肠癌的治疗中多数Ⅱ期患者不需要化疗,而在Ⅲ期患者,尽管我们知道其中有不同预后的亚组,但目前还是尽量给予(新)辅助治疗。随着证据的积累,高位直肠癌的治疗策略能否向结肠癌“靠近”——手术确认为Ⅱ期的患者可以不需要辅助治疗?这是非常重要的问题。此外,如果有足够多的病例数,FOWARC研究中新辅助降期但没有达到pCR的那部分Ⅱ期患者的转归也会很值得关注。
FOWARC研究很独特的一点是,FOLFOX-RT组患者先给予FOLFOX化疗然后放化疗,FOLFOX组的患者大多数只接受了FOLFOX化疗而没有接受放疗。FOLFOX组的pCR率较另外两组低,但是3组的R0切除率相似。因此,在数据成熟之后,LRR就会非常关键。如果FOLFOX组与FOLFOX-RT组的LRR相似,那么结果就会变得非常有意思,值得进行更大规模的研究。
FOWARC研究的必要性还在于,来自亚洲的研究数据可能会帮助我们更好地了解疾病的地域差异,同时,我们也需要了解来自于不同国家的不同治疗策略。总之,这是一个非常合适的研究,可以为未来更多的研究提供重要信息。(注:Benson教授为NCCN理事会成员、NCCN结直肠癌专家委员会主席)
■链接·参与FOWARC研究的中心
中山大学附属第六医院、福建医科大学附属协和医院、上海交通大学医学院附属新华医院、华中科技大学同济医学院附属协和医院、广州市第一人民医院、中山大学附属第三医院、佛山市第一人民医院、南方医科大学珠江医院、广东省人民医院、上海交通大学医学院附属瑞金医院、湖南省人民医院、厦门大学附属第一医院、广州军区总医院、广州医科大学附属第二医院、东莞康华医院
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#手术期#
107
#ASC#
78
期待
133
看看
167
期待结果
108
#FOLFOX#
53
#mFOLFOX6#
76