冠心病患者伴非酒精性脂肪肝的临床转归
2012-09-07 庄云芳 中国医学论坛报
文章作者:北京大学人民医院 陈云超 刘玉兰 非酒精性脂肪肝(NAFLD)与冠心病概况 NAFLD包括非酒精性单纯性脂肪肝、非酒精性脂肪性肝炎及其相关肝硬化和肝细胞癌。近来,NAFLD的发病率呈明显上升趋势,已成为发达国家第一大慢性肝病及肝功能异常的首要病因,普通成年人患病率为17%~33%。 &
非酒精性脂肪肝(NAFLD)与冠心病概况 NAFLD包括非酒精性单纯性脂肪肝、非酒精性脂肪性肝炎及其相关肝硬化和肝细胞癌。近来,NAFLD的发病率呈明显上升趋势,已成为发达国家第一大慢性肝病及肝功能异常的首要病因,普通成年人患病率为17%~33%。
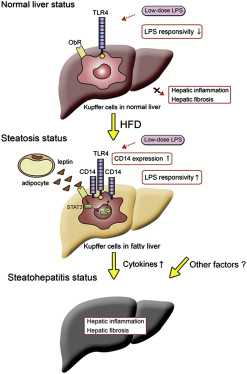
NAFLD目前被认为是代谢综合征的一部分,而代谢综合征是导致糖尿病、心脑血管疾病的危险因素,日益增多的脂肪肝主要与胰岛素抵抗密切相关,且NAFLD患者对许多药物和毒物的敏感性增加。对于NAFLD的发病机制,目前经典的理论是“二次打击”学说:“第一次打击”是指脂肪储积,“第二次打击”是指氧化应激和异常细胞因子的作用导致肝脏坏死性炎症和纤维化。
冠状动脉粥样硬化性心脏病与冠状动脉功能改变一起统称为冠状动脉性心脏病,简称冠心病。随着我国人口老龄化和人民生活水平的逐步提高,冠心病的发病率呈快速上升趋势,占心脏病死亡数的10%~20%,且中年及青年人群发病人数有所增加。冠心病已成为常见病、多发病,严重威胁人类健康。冠心病是多病因的疾病,即多种因素作用于不同环节所致,这些因素称为危险因素,包括如年龄、性别、饮酒、吸烟、精神紧张、A型性格、高血压、糖尿病、血脂异常、超重和肥胖等。
NAFLD与冠心病的关系及临床转归 近来国外学者发现NAFLD患者中合并冠心病的比例高于其他人群,并认为NAFLD是冠心病的独立危险因素之一。部分研究结果提示NAFLD患者冠心病的发病率和死亡率升高。由于NAFLD与低高密度脂蛋白、高甘油三酯血症、肥胖、糖尿病等冠心病危险因素密切相关,因而NAFLD与冠心病间的联系受到广泛关注。目前研究发现,NAFLD可能通过多个方面对冠状动脉粥样硬化性心脏病产生影响。
NAFLD可能通过多个方面对冠心病产生影响:
1. 血脂异常:NAFLD患者甘油三酯、胆固醇、低密度脂蛋白(LDL)水平明显升高,而在冠心病众多危险因素中,血脂异常是目前被公认的重要危险因素。众多 研究均提示LDL升高是冠心病的主要病因,降低LDL治疗能降低近期心脏病危险达40%余,还可能降低10年或更久的远期危险。
2. 代谢综合征:代谢综合征最主要表现为高脂血症、肥胖、2型糖尿病,甘油三酯及胆固醇升高是脂肪肝的血脂表现特点,脂肪肝引起冠心病的机理与甘油三酯、胆固 醇增高、高密度脂蛋白降低有关,高脂血症被公认为是致动脉粥样硬化的危险因素,高脂血症诱发脂肪肝的同时,也易引发高血压和冠心病。
3.脂联素:肝细胞脂肪变后具有了部分脂肪细胞的功能,脂联素是最主要由脂肪细胞分泌的激素,研究发现其与动脉粥样硬化的形成密切相关,而肝脏脂肪变导致脂肪激素分泌增多,这些增多的激素可能将脂肪肝与动脉粥样硬化联系起来。
NAFLD与冠心病有共同的危险因素,在当前NAFLD及冠心病发病率不断升高的情况下,无论从肝病还是动脉硬化和心血管疾病的角度,均应高度重视NAFLD的防治,在防治中宜采用对多种危险因素联合的干预策略。
目前认为,改变饮食和生活习惯、减少其他危险因素可有效减少或避免疾病发生。定期体检和问卷调查有利于发现NAFLD高危人群及危险因素,并对体检者NAFLD的患病风险进行预测,也可早期诊断NAFLD,更重要的是,可在此基础上对NAFLD高危人群和患者进行长期有针对性的健康干预,如开展健康教育,提倡健康生活方式,调整营养结构、平衡膳食,制订健康促进计划、推广健身运动、控制体重,定期健康检查等跟踪随访并定期评估干预效果以及调整计划等。以提高全民的健康水平,同时积极对上述人群进行心血管事件评估,争取尽早发现,尽早干预。
NAFID治疗策略
鉴于NAFLD与代谢综合征密切相关,互为独立的危险因素, 因此NAFLD的治疗强调综合治疗和基础治疗的重要性,尤其不能忽视针对肝脏损伤的治疗。
2010年《非酒精性脂肪性肝病诊疗指南》明确指出,NAFLD伴肝功能异常、代谢综合征、2型糖尿病者,肝活检确诊非酒精性脂肪性肝炎者以及基础用药或合并用药可能诱发肝损害者,可合理选用保肝药治疗,如多烯磷脂酰胆碱等。
多烯磷脂酰胆碱的结构与内源性磷脂相似,具有修复肝细胞生物膜、调节脂质代谢、抗氧化、抗纤维化及抗细胞凋亡等多重作用,在多项大型临床研究中已显示其可有效改善NAFLD,目前已成为国内临床诊疗指南推荐的保肝、护肝药物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#酒精性#
85
#临床转归#
100
#非酒精性#
94
#酒精性脂肪肝#
86
#冠心病患者#
105